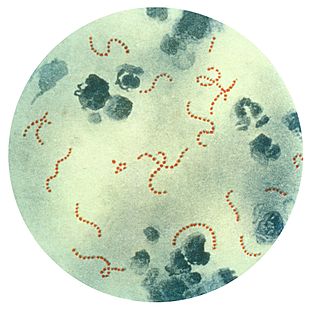
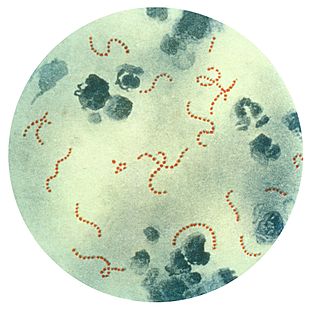
Streptococcus is a genus of gram-positive or spherical bacteria that belongs to the family Streptococcaceae, within the order Lactobacillales, in the phylum Bacillota. Cell division in streptococci occurs along a single axis, thus when growing they tend to form pairs or chains, which may appear bent or twisted. This differs from staphylococci, which divide along multiple axes, thereby generating irregular, grape-like clusters of cells. Most streptococci are oxidase-negative and catalase-negative, and many are facultative anaerobes.

Group A streptococcal infections are a number of infections with Streptococcus pyogenes, a group A streptococcus (GAS). S. pyogenes is a species of beta-hemolytic Gram-positive bacteria that is responsible for a wide range of infections that are mostly common and fairly mild. If the bacteria enters the bloodstream, the infection can become severe and life-threatening, and is called an invasive GAS (iGAS).

Scarlet fever, also known as scarlatina, is an infectious disease caused by Streptococcus pyogenes, a Group A streptococcus (GAS). It most commonly affects children between five and 15 years of age. The signs and symptoms include a sore throat, fever, headache, swollen lymph nodes, and a characteristic rash. The face is flushed and the rash is red and blanching. It typically feels like sandpaper and the tongue may be red and bumpy. The rash occurs as a result of capillary damage by exotoxins produced by S.pyogenes. On darker-pigmented skin the rash may be hard to discern.

Streptococcal pharyngitis, also known as streptococcal sore throat, is pharyngitis caused by Streptococcus pyogenes, a gram-positive, group A streptococcus. Common symptoms include fever, sore throat, red tonsils, and enlarged lymph nodes in the front of the neck. A headache and nausea or vomiting may also occur. Some develop a sandpaper-like rash which is known as scarlet fever. Symptoms typically begin one to three days after exposure and last seven to ten days.

Pharyngitis is inflammation of the back of the throat, known as the pharynx. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, difficulty swallowing, swollen lymph nodes, and a hoarse voice. Symptoms usually last 3–5 days, but can be longer depending on cause. Complications can include sinusitis and acute otitis media. Pharyngitis is a type of upper respiratory tract infection.

Rheumatic fever (RF) is an inflammatory disease that can involve the heart, joints, skin, and brain. The disease typically develops two to four weeks after a streptococcal throat infection. Signs and symptoms include fever, multiple painful joints, involuntary muscle movements, and occasionally a characteristic non-itchy rash known as erythema marginatum. The heart is involved in about half of the cases. Damage to the heart valves, known as rheumatic heart disease (RHD), usually occurs after repeated attacks but can sometimes occur after one. The damaged valves may result in heart failure, atrial fibrillation and infection of the valves.

Chorea is an abnormal involuntary movement disorder, characterized by quick movements of the hands or feet. It is one of a group of neurological disorders called dyskinesias. The term chorea is derived from Ancient Greek χορεία (choreia) 'dance', as the movements of the body is comparable to dancing.

Tonsillitis is inflammation of the tonsils in the upper part of the throat. It can be acute or chronic. Acute tonsillitis typically has a rapid onset. Symptoms may include sore throat, fever, enlargement of the tonsils, trouble swallowing, and enlarged lymph nodes around the neck. Complications include peritonsillar abscess (quinsy).

Erythema marginatum is an acquired skin condition which primarily affects the arms, trunk, and legs. It is a type of erythema characterised by bright pink or red circular lesions which have sharply-defined borders and faint central clearing. The lesions typically range from 3 to 10 cm in size, and are distributed symmetrically over the torso and inner surfaces of the limbs and extensor surfaces. The lesions last between one and four weeks but have been known to be present on patients for as long as several months.
A complication in medicine, or medical complication, is an unfavorable result of a disease, health condition, or treatment. Complications may adversely affect the prognosis, or outcome, of a disease. Complications generally involve a worsening in the severity of the disease or the development of new signs, symptoms, or pathological changes that may become widespread throughout the body and affect other organ systems. Thus, complications may lead to the development of new diseases resulting from previously existing diseases. Complications may also arise as a result of various treatments.

Cryoglobulinemia is a medical condition in which the blood contains large amounts of pathological cold sensitive antibodies called cryoglobulins – proteins – that become insoluble at reduced temperatures. This should be contrasted with cold agglutinins, which cause agglutination of red blood cells.
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS) is a controversial hypothetical diagnosis for a subset of children with rapid onset of obsessive-compulsive disorder (OCD) or tic disorders. Symptoms are proposed to be caused by group A streptococcal (GAS), and more specifically, group A beta-hemolytic streptococcal (GABHS) infections. OCD and tic disorders are hypothesized to arise in a subset of children as a result of a post-streptococcal autoimmune process. The proposed link between infection and these disorders is that an autoimmune reaction to infection produces antibodies that interfere with basal ganglia function, causing symptom exacerbations, and this autoimmune response results in a broad range of neuropsychiatric symptoms.

Neurosyphilis is the infection of the central nervous system in a patient with syphilis. In the era of modern antibiotics, the majority of neurosyphilis cases have been reported in HIV-infected patients. Meningitis is the most common neurological presentation in early syphilis. Tertiary syphilis symptoms are exclusively neurosyphilis, though neurosyphilis may occur at any stage of infection.
Causes and origins of Tourette syndrome have not been fully elucidated. Tourette syndrome is an inherited neurodevelopmental disorder that begins in childhood or adolescence, characterized by the presence of multiple motor tics and at least one phonic tic, which characteristically wax and wane. Tourette's syndrome occurs along a spectrum of tic disorders, which includes transient tics and chronic tics.
Chorea gravidarum is a rare type of chorea which presents with involuntary abnormal movement, characterized by abrupt, brief, nonrhythmic, nonrepetitive movement of any limb, often associated with nonpatterned facial grimaces. It is a complication of pregnancy which can be associated with eclampsia and its effects upon the basal ganglia. It is not a causal or pathologically distinct entity but a generic term for chorea of any cause starting during pregnancy. It is associated with history of Sydenham's chorea. It mostly occurs in young patients; the average age is 22 years.
Neuroborreliosis is a disorder of the central nervous system. A neurological manifestation of Lyme disease, neuroborreliosis is caused by a systemic infection of spirochetes of the genus Borrelia. Symptoms of the disease include erythema migrans and flu-like symptoms.

Lupus, technically known as systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms.

Basal ganglia disease is a group of physical problems that occur when the group of nuclei in the brain known as the basal ganglia fail to properly suppress unwanted movements or to properly prime upper motor neuron circuits to initiate motor function. Research indicates that increased output of the basal ganglia inhibits thalamocortical projection neurons. Proper activation or deactivation of these neurons is an integral component for proper movement. If something causes too much basal ganglia output, then the ventral anterior (VA) and ventral lateral (VL) thalamocortical projection neurons become too inhibited, and one cannot initiate voluntary movement. These disorders are known as hypokinetic disorders. However, a disorder leading to abnormally low output of the basal ganglia leads to reduced inhibition, and thus excitation, of the thalamocortical projection neurons which synapse onto the cortex. This situation leads to an inability to suppress unwanted movements. These disorders are known as hyperkinetic disorders.
Perianal cellulitis, also known as perianitis or perianal streptococcal dermatitis, is a bacterial infection affecting the lower layers of the skin (cellulitis) around the anus. It presents as bright redness in the skin and can be accompanied by pain, difficulty defecating, itching, and bleeding. This disease is considered a complicated skin and soft tissue infection (cSSTI) because of the involvement of the deeper soft tissues.

Vogt–Koyanagi–Harada disease (VKH) is a multisystem disease of presumed autoimmune cause that affects melanin-pigmented tissues. The most significant manifestation is bilateral, diffuse uveitis, which affects the eyes. VKH may variably also involve the inner ear, with effects on hearing, the skin, and the meninges of the central nervous system.