Related Research Articles

Glaucoma is a group of eye diseases that can lead to damage of the optic nerve. The optic nerve transmits visual information from the eye to the brain. Glaucoma may cause vision loss if left untreated. It has been called the "silent thief of sight" because the loss of vision usually occurs slowly over a long period of time. A major risk factor for glaucoma is increased pressure within the eye, known as intraocular pressure (IOP). It is associated with old age, a family history of glaucoma, and certain medical conditions or the use of some medications. The word glaucoma comes from the Ancient Greek word γλαυκός, meaning 'gleaming, blue-green, gray'.

Pilocarpine is a lactone alkaloid originally extracted from plants of the Pilocarpus genus. It is used as a medication to reduce pressure inside the eye and treat dry mouth. As an eye drop it is used to manage angle closure glaucoma until surgery can be performed, ocular hypertension, primary open angle glaucoma, and to constrict the pupil after dilation. However, due to its side effects, it is no longer typically used for long-term management. Onset of effects with the drops is typically within an hour and lasts for up to a day. By mouth it is used for dry mouth as a result of Sjögren syndrome or radiation therapy.

The ciliary body is a part of the eye that includes the ciliary muscle, which controls the shape of the lens, and the ciliary epithelium, which produces the aqueous humor. The aqueous humor is produced in the non-pigmented portion of the ciliary body. The ciliary body is part of the uvea, the layer of tissue that delivers oxygen and nutrients to the eye tissues. The ciliary body joins the ora serrata of the choroid to the root of the iris.

Intraocular pressure (IOP) is the fluid pressure inside the eye. Tonometry is the method eye care professionals use to determine this. IOP is an important aspect in the evaluation of patients at risk of glaucoma. Most tonometers are calibrated to measure pressure in millimeters of mercury (mmHg).
Betaxolol is a selective beta1 receptor blocker used in the treatment of hypertension and angina. It is also a adrenergic blocker with no partial agonist action and minimal membrane stabilizing activity. Being selective for beta1 receptors, it typically has fewer systemic side effects than non-selective beta-blockers, for example, not causing bronchospasm as timolol may. Betaxolol also shows greater affinity for beta1 receptors than metoprolol. In addition to its effect on the heart, betaxolol reduces the pressure within the eye. This effect is thought to be caused by reducing the production of the liquid within the eye. The precise mechanism of this effect is not known. The reduction in intraocular pressure reduces the risk of damage to the optic nerve and loss of vision in patients with elevated intraocular pressure due to glaucoma.

Latanoprost, sold under the brand name Xalatan among others, is a medication used to treat increased pressure inside the eye. This includes ocular hypertension and open-angle glaucoma. Latanaprost is applied as eye drops to the eyes. Onset of effects is usually within four hours, and they last for up to a day.

Tonometry is the procedure that eye care professionals perform to determine the intraocular pressure (IOP), the fluid pressure inside the eye. It is an important test in the evaluation of patients at risk from glaucoma. Most tonometers are calibrated to measure pressure in millimeters of mercury (mmHg), with the normal eye pressure range between 10 and 21 mmHg (13–28 hPa).

Schlemm's canal, also known as the canal of Schlemm, and as the scleral venous sinus, is a circular lymphatic-like vessel in the eye. It collects aqueous humor from the anterior chamber and delivers it into the episcleral blood vessels. Canaloplasty may be used to widen it.
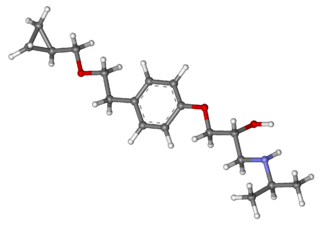
Brimonidine is an α2 agonist medication used to treat open-angle glaucoma, ocular hypertension, and rosacea. In rosacea it improves the redness. It is used as eye drops or applied to the skin. It is also available in the fixed-dose combination medication brimonidine/timolol along with timolol maleate.

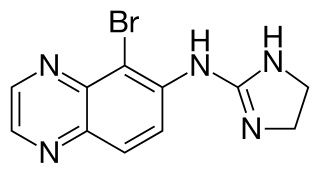
Apraclonidine (INN), also known under the brand name Iopidine, is a sympathomimetic used in glaucoma therapy. It is an α2 adrenergic receptor agonist and a weak α1 adrenergic receptor agonist.

Glaucoma is a group of diseases affecting the optic nerve that results in vision loss and is frequently characterized by raised intraocular pressure (IOP). There are many glaucoma surgeries, and variations or combinations of those surgeries, that facilitate the escape of excess aqueous humor from the eye to lower intraocular pressure, and a few that lower IOP by decreasing the production of aqueous humor.
Brimonidine/timolol, sold under the brand name Combigan among others, is a fixed-dose combination medication eye drop used for the treatment of glaucoma. It is a combination of brimonidine and timolol.
Pseudoexfoliation syndrome, often abbreviated as PEX and sometimes as PES or PXS, is an aging-related systemic disease manifesting itself primarily in the eyes which is characterized by the accumulation of microscopic granular amyloid-like protein fibers. Its cause is unknown, although there is speculation that there may be a genetic basis. It is more prevalent in women than men, and in persons past the age of seventy. Its prevalence in different human populations varies; for example, it is prevalent in Scandinavia. The buildup of protein clumps can block normal drainage of the eye fluid called the aqueous humor and can cause, in turn, a buildup of pressure leading to glaucoma and loss of vision. As worldwide populations become older because of shifts in demography, PEX may become a matter of greater concern.
Trabeculoplasty is a laser treatment for glaucoma. It is done on an argon laser equipped slit lamp, using a Goldmann gonioscope lens mirror. Specifically, an argon laser is used to improve drainage through the eye's trabecular meshwork, from which the aqueous humour drains. This helps reduce intraocular pressure caused by open-angle glaucoma.

Canine glaucoma refers to a group of diseases in dogs that affect the optic nerve and involve a loss of retinal ganglion cells in a characteristic pattern. An intraocular pressure greater than 22 mmHg (2.9 kPa) is a significant risk factor for the development of glaucoma. Untreated glaucoma in dogs leads to permanent damage of the optic nerve and resultant visual field loss, which can progress to blindness.
Micro-invasive glaucoma surgery (MIGS) is the latest advance in surgical treatment for glaucoma, which aims to reduce intraocular pressure by either increasing outflow of aqueous humor or reducing its production. MIGS comprises a group of surgical procedures which share common features. MIGS procedures involve a minimally invasive approach, often with small cuts or micro-incisions through the cornea that causes the least amount of trauma to surrounding scleral and conjunctival tissues. The techniques minimize tissue scarring, allowing for the possibility of traditional glaucoma procedures such as trabeculectomy or glaucoma valve implantation to be performed in the future if needed.

Secondary glaucoma is a collection of progressive optic nerve disorders associated with a rise in intraocular pressure (IOP) which results in the loss of vision. In clinical settings, it is defined as the occurrence of IOP above 21 mmHg requiring the prescription of IOP-managing drugs. It can be broadly divided into two subtypes: secondary open-angle glaucoma and secondary angle-closure glaucoma, depending on the closure of the angle between the cornea and the iris. Principal causes of secondary glaucoma include optic nerve trauma or damage, eye disease, surgery, neovascularization, tumours and use of steroid and sulfa drugs. Risk factors for secondary glaucoma include uveitis, cataract surgery and also intraocular tumours. Common treatments are designed according to the type and the underlying causative condition, in addition to the consequent rise in IOP. These include drug therapy, the use of miotics, surgery or laser therapy.

Uveitic glaucoma is most commonly a progression stage of noninfectious anterior uveitis or iritis.
Ocular hypotony, or ocular hypotension, or shortly hypotony, is the medical condition in which intraocular pressure (IOP) of the eye is very low.
Hypotony maculopathy is maculopathy due to very low intraocular pressure known as ocular hypotony. Maculopathy occurs either due to increased outflow of aqueous humor through angle of anterior chamber or less commonly, due to decreased aqueous humor secretion by ciliary body.
References
- ↑ "Ocular Hypertension, Glaucoma & Eye Drops" (PDF). American Academy of Ophthalmology. June 2002. Archived from the original (PDF) on 25 November 2005.
- ↑ "Ocular Hypertension". American Optometric Association.
- ↑ "Tonometry". webMD.
- 1 2 3 4 Clement Freiberg, Josefine; von Spreckelsen, Alexander; Kolko, Miriam; Azuara-Blanco, Augusto; Virgili, Gianni (2022-06-10). Cochrane Eyes and Vision Group (ed.). "Rho kinase inhibitor for primary open-angle glaucoma and ocular hypertension". Cochrane Database of Systematic Reviews. 2022 (6). doi:10.1002/14651858.CD013817.pub2. PMC 9185806 . PMID 35686679.
- ↑ "Glaucoma Overview". eMedicine. Archived from the original on 2008-07-04. Retrieved 2005-12-28.
- ↑ "Aqueous and Vitreous Humor: Anatomy, Function & Location". Cleveland Clinic. Archived from the original on 2024-10-05. Retrieved 2024-12-13.
- ↑ "Ocular Hypertension". Yale Medicine. Retrieved 2024-12-13.
- ↑ "Ocular Hypertension". Yale Medicine. Retrieved 2024-12-13.
- 1 2 Salmon, John F. (2020). "Glaucoma". Kanski's clinical ophthalmology : a systematic approach (9th ed.). Edinburgh: Elsevier. ISBN 978-0-7020-7713-5. OCLC 1131846767.
- ↑ "Moran CORE | Ocular Hypertension" . Retrieved 2024-12-18.
- ↑ "Eye (Intraocular) Pressure: What It Is & How It's Measured". Cleveland Clinic. Archived from the original on 2024-12-07. Retrieved 2024-12-13.
- ↑ Bader, John; Zeppieri, Marco; Havens, Shane J. (2024), "Tonometry", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29630277 , retrieved 2024-12-13
- ↑ "Ocular Hypertension". Yale Medicine. Retrieved 2024-12-18.
- ↑ "Moran CORE | Ocular Hypertension" . Retrieved 2024-12-18.
- ↑ "Moran CORE | Ocular Hypertension" . Retrieved 2024-12-18.
- 1 2 Rolim-de-Moura, Christiane R; Paranhos Jr, Augusto; Loutfi, Mohamed; Burton, David; Wormald, Richard; Evans, Jennifer R (2022-08-09). Cochrane Eyes and Vision Group (ed.). "Laser trabeculoplasty for open-angle glaucoma and ocular hypertension". Cochrane Database of Systematic Reviews. 2022 (8). doi:10.1002/14651858.CD003919.pub3. PMC 9361429 . PMID 35943114.
- ↑ Grossman, Adriana L.; Javitt, Matthew J.; Moster, Steven J.; Grajewski, Alana L.; Beck, Allen D.; Blieden, Lauren S.; Bitrian, Elena; Chang, Ta C.; Freedman, Sharon F.; Hodapp, Elizabeth; Joos, Keren M.; Reiser, Bibiana J.; Tanna, Angelo P. (2019-11-01). "American Glaucoma Society Position Statement on Cannabinoid Use in Pediatric Glaucoma Patients". Ophthalmology Glaucoma. 2 (6): 365–366. doi:10.1016/j.ogla.2019.07.007. ISSN 2589-4196.
- ↑ Jampel H (February 2010). "American glaucoma society position statement: marijuana and the treatment of glaucoma". Journal of Glaucoma. 19 (2): 75–76. doi:10.1097/ijg.0b013e3181d12e39. PMID 20160576.
- ↑ "What Is Ocular Hypertension?". American Academy of Ophthalmology. 2024-09-26. Retrieved 2024-12-16.
- ↑ Gordon, Mae O.; Kass, Michael A. (2018-05-01). "What We Have Learned From the Ocular Hypertension Treatment Study". American Journal of Ophthalmology. 189: xxiv–xxvii. doi:10.1016/j.ajo.2018.02.016. ISSN 0002-9394.
- ↑ Gordon, Mae O.; Kass, Michael A. (2018-05-01). "What We Have Learned From the Ocular Hypertension Treatment Study". American Journal of Ophthalmology. 189: xxiv–xxvii. doi:10.1016/j.ajo.2018.02.016. ISSN 0002-9394.
- ↑ "Clinical Trials in Glaucoma - EyeWiki". eyewiki.org. Retrieved 2024-12-16.
- ↑ "Clinical Trials in Glaucoma - EyeWiki". eyewiki.org. Retrieved 2024-12-16.
- ↑ "Clinical Trials in Glaucoma - EyeWiki". eyewiki.org. Retrieved 2024-12-16.
- ↑ "Clinical Trials in Glaucoma - EyeWiki". eyewiki.org. Retrieved 2024-12-16.
- ↑ Gazzard G, Konstantakopoulou E, Garway-Heath D, Garg A, Vickerstaff V, Hunter R, et al. (April 2019). "Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial". Lancet. 393 (10180): 1505–1516. doi:10.1016/S0140-6736(18)32213-X. PMC 6495367 . PMID 30862377.; Lay summary in: "A laser eye procedure can be effective and safe if used early as treatment for glaucoma". NIHR Evidence. National Institute for Health and Care Research. 4 June 2019. doi:10.3310/signal-000774.
Plain English summary