Vaccination is the administration of a vaccine to help the immune system develop immunity from a disease. Vaccines contain a microorganism or virus in a weakened, live or killed state, or proteins or toxins from the organism. In stimulating the body's adaptive immunity, they help prevent sickness from an infectious disease. When a sufficiently large percentage of a population has been vaccinated, herd immunity results. Herd immunity protects those who may be immunocompromised and cannot get a vaccine because even a weakened version would harm them. The effectiveness of vaccination has been widely studied and verified. Vaccination is the most effective method of preventing infectious diseases; widespread immunity due to vaccination is largely responsible for the worldwide eradication of smallpox and the elimination of diseases such as polio and tetanus from much of the world. However, some diseases, such as measles outbreaks in America, have seen rising cases due to relatively low vaccination rates in the 2010s – attributed, in part, to vaccine hesitancy. According to the World Health Organization, vaccination prevents 3.5–5 million deaths per year.

A vaccine is a biological preparation that provides active acquired immunity to a particular infectious or malignant disease. The safety and effectiveness of vaccines has been widely studied and verified. A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as a threat, destroy it, and to further recognize and destroy any of the microorganisms associated with that agent that it may encounter in the future.

Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Antiviral drugs are one class of antimicrobials, a larger group which also includes antibiotic, antifungal and antiparasitic drugs, or antiviral drugs based on monoclonal antibodies. Most antivirals are considered relatively harmless to the host, and therefore can be used to treat infections. They should be distinguished from virucides, which are not medication but deactivate or destroy virus particles, either inside or outside the body. Natural virucides are produced by some plants such as eucalyptus and Australian tea trees.

Herd immunity is a form of indirect protection that applies only to contagious diseases. It occurs when a sufficient percentage of a population has become immune to an infection, whether through previous infections or vaccination, thereby reducing the likelihood of infection for individuals who lack immunity.
Asplenia refers to the absence of normal spleen function and is associated with some serious infection risks. Hyposplenism is used to describe reduced ('hypo-') splenic functioning, but not as severely affected as with asplenism.

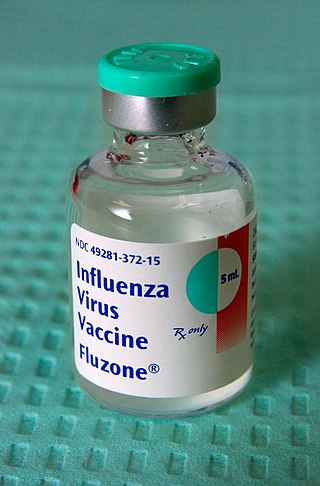
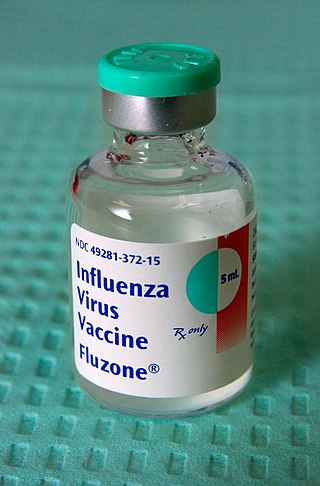
Influenza vaccines, also known as flu shots, are vaccines that protect against infection by influenza viruses. New versions of the vaccines are developed twice a year, as the influenza virus rapidly changes. While their effectiveness varies from year to year, most provide modest to high protection against influenza. The United States Centers for Disease Control and Prevention (CDC) estimates that vaccination against influenza reduces sickness, medical visits, hospitalizations, and deaths. Immunized workers who do catch the flu return to work half a day sooner on average. Vaccine effectiveness in those over 65 years old remains uncertain due to a lack of high-quality research.

Vaccine hesitancy is a delay in acceptance, or refusal, of vaccines despite the availability of vaccine services and supporting evidence. The term covers refusals to vaccinate, delaying vaccines, accepting vaccines but remaining uncertain about their use, or using certain vaccines but not others. The scientific consensus that vaccines are generally safe and effective is overwhelming. Vaccine hesitancy often results in disease outbreaks and deaths from vaccine-preventable diseases. Therefore, the World Health Organization characterizes vaccine hesitancy as one of the top ten global health threats.

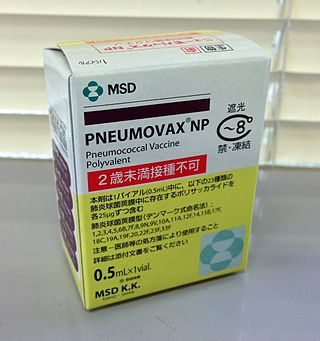
Pneumococcal polysaccharide vaccine, sold under the brand name Pneumovax 23, is a pneumococcal vaccine that is used for the prevention of pneumococcal disease caused by the 23 serotypes of Streptococcus pneumoniae contained in the vaccine as capsular polysaccharides. It is given by intramuscular or subcutaneous injection.

The number needed to treat (NNT) or number needed to treat for an additional beneficial outcome (NNTB) is an epidemiological measure used in communicating the effectiveness of a health-care intervention, typically a treatment with medication. The NNT is the average number of patients who need to be treated to prevent one additional bad outcome. It is defined as the inverse of the absolute risk reduction, and computed as , where is the incidence in the treated (exposed) group, and is the incidence in the control (unexposed) group. This calculation implicitly assumes monotonicity, that is, no individual can be harmed by treatment. The modern approach, based on counterfactual conditionals, relaxes this assumption and yields bounds on NNT.

Meningococcal disease describes infections caused by the bacterium Neisseria meningitidis. It has a high mortality rate if untreated but is vaccine-preventable. While best known as a cause of meningitis, it can also result in sepsis, which is an even more damaging and dangerous condition. Meningitis and meningococcemia are major causes of illness, death, and disability in both developed and under-developed countries.

Pneumococcal conjugate vaccine is a pneumococcal vaccine and a conjugate vaccine used to protect infants, young children, and adults against disease caused by the bacterium Streptococcus pneumoniae (pneumococcus). It contains purified capsular polysaccharide of pneumococcal serotypes conjugated to a carrier protein to improve antibody response compared to the pneumococcal polysaccharide vaccine. The World Health Organization (WHO) recommends the use of the conjugate vaccine in routine immunizations given to children.
A breakthrough infection is a case of illness in which a vaccinated individual becomes infected with the illness, because the vaccine has failed to provide complete immunity against the pathogen. Breakthrough infections have been identified in individuals immunized against a variety of diseases including mumps, varicella (Chickenpox), influenza, and COVID-19. The characteristics of the breakthrough infection are dependent on the virus itself. Often, infection of the vaccinated individual results in milder symptoms and shorter duration than if the infection were contracted naturally.
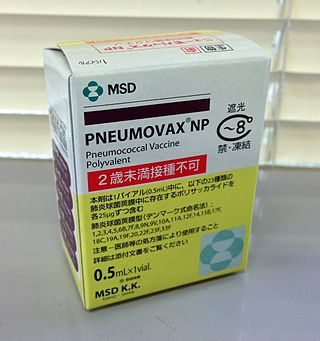
Pneumococcal vaccines are vaccines against the bacterium Streptococcus pneumoniae. Their use can prevent some cases of pneumonia, meningitis, and sepsis. There are two types of pneumococcal vaccines: conjugate vaccines and polysaccharide vaccines. They are given by injection either into a muscle or just under the skin.
Vaccine efficacy or vaccine effectiveness is the percentage reduction of disease cases in a vaccinated group of people compared to an unvaccinated group. For example, a vaccine efficacy or effectiveness of 80% indicates an 80% decrease in the number of disease cases among a group of vaccinated people compared to a group in which nobody was vaccinated. When a study is carried out using the most favorable, ideal or perfectly controlled conditions, such as those in a clinical trial, the term vaccine efficacy is used. On the other hand, when a study is carried out to show how well a vaccine works when they are used in a bigger, typical population under less-than-perfectly controlled conditions, the term vaccine effectiveness is used.
A vaccination policy is a health policy adopted in order to prevent the spread of infectious disease. These policies are generally put into place by State or local governments, but may also be set by private facilities, such as workplaces or schools. Many policies have been developed and implemented since vaccines were first made widely available.
Mass vaccination is a public policy effort to vaccinate a large number of people, possibly the entire population of the world or of a country or region, within a short period of time. This policy may be directed during a pandemic, when there is a localized outbreak or scare of a disease for which a vaccine exists, or when a new vaccine is invented.

Pandemrix is an influenza vaccine for influenza pandemics, such as the 2009 flu pandemic. The vaccine was developed by GlaxoSmithKline (GSK) and patented in September 2006.

The 2009 swine flu pandemic vaccines were influenza vaccines developed to protect against the pandemic H1N1/09 virus. These vaccines either contained inactivated (killed) influenza virus, or weakened live virus that could not cause influenza. The killed virus was injected, while the live virus was given as a nasal spray. Both these types of vaccine were produced by growing the virus in chicken eggs. Around three billion doses were produced, with delivery in November 2009.

Targeted immunization strategies are approaches designed to increase the immunization level of populations and decrease the chances of epidemic outbreaks. Though often in regards to use in healthcare practices and the administration of vaccines to prevent biological epidemic outbreaks, these strategies refer in general to immunization schemes in complex networks, biological, social or artificial in nature. Identification of at-risk groups and individuals with higher odds of spreading the disease often plays an important role in these strategies, since targeted immunization in high-risk groups is necessary for effective eradication efforts and has a higher return on investment than immunizing larger but lower-risk groups.

Shabir Ahmed Madhi is a South African physician who is professor of vaccinology and director of the South African Medical Research Council Respiratory and Meningeal Pathogens Research Unit at the University of the Witwatersrand, and National Research Foundation/Department of Science and Technology Research Chair in Vaccine Preventable Diseases. In January 2021, he was appointed Dean of the Faculty of Health Sciences at the University of the Witwateratand.