The foot is an anatomical structure found in many vertebrates. It is the terminal portion of a limb which bears weight and allows locomotion. In many animals with feet, the foot is a separate organ at the terminal part of the leg made up of one or more segments or bones, generally including claws and/or nails.

The leg is the entire lower limb of the human body, including the foot, thigh or sometimes even the hip or buttock region. The major bones of the leg are the femur, tibia, and adjacent fibula.

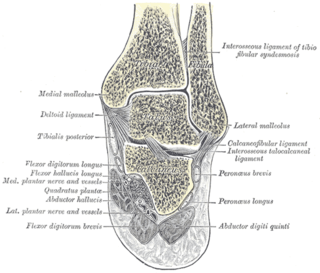
The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates ; it connects the knee with the ankle. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body, after the femur. The leg bones are the strongest long bones as they support the rest of the body.

The fibula or calf bone is a leg bone on the lateral side of the tibia, to which it is connected above and below. It is the smaller of the two bones and, in proportion to its length, the most slender of all the long bones. Its upper extremity is small, placed toward the back of the head of the tibia, below the knee joint and excluded from the formation of this joint. Its lower extremity inclines a little forward, so as to be on a plane anterior to that of the upper end; it projects below the tibia and forms the lateral part of the ankle joint.

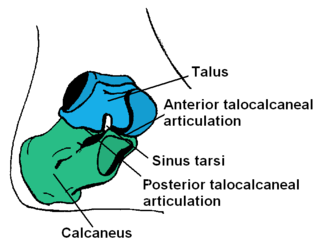
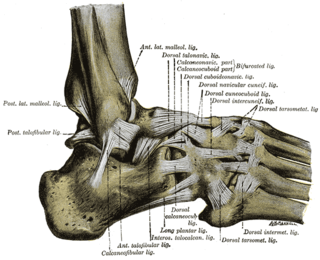
The ankle, the talocrural region or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.
Pott's fracture, also known as Pott's syndrome I and Dupuytren fracture, is an archaic term loosely applied to a variety of bimalleolar ankle fractures. The injury is caused by a combined abduction external rotation from an eversion force. This action strains the sturdy medial (deltoid) ligament of the ankle, often tearing off the medial malleolus due to its strong attachment. The talus then moves laterally, shearing off the lateral malleolus or, more commonly, breaking the fibula superior to the tibiofibular syndesmosis. If the tibia is carried anteriorly, the posterior margin of the distal end of the tibia is also sheared off by the talus. A fractured fibula in addition to detaching the medial malleolus will tear the tibiofibular syndesmosis. The combined fracture of the medial malleolus, lateral malleolus, and the posterior margin of the distal end of the tibia is known as a "trimalleolar fracture".

A syndesmosis is a type of fibrous joint in which two parallel bones are united to each other by fibrous connective tissue. The gap between the bones may be narrow, with the bones joined by ligaments, or the gap may be wide and filled in by a broad sheet of connective tissue called an interosseous membrane. The syndesmoses found in the forearm and leg serve to unite parallel bones and prevent their separation.
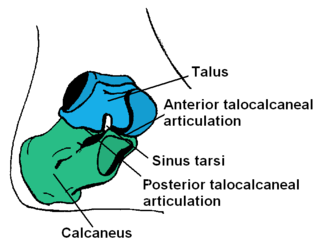
The talus, talus bone, astragalus, or ankle bone is one of the group of foot bones known as the tarsus. The tarsus forms the lower part of the ankle joint. It transmits the entire weight of the body from the lower legs to the foot.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.

The inferior tibiofibular joint, also known as the distal tibiofibular joint, is formed by the rough, convex surface of the medial side of the distal end of the fibula, and a rough concave surface on the lateral side of the tibia.

The superior tibiofibular articulation is an arthrodial joint between the lateral condyle of tibia and the head of the fibula.
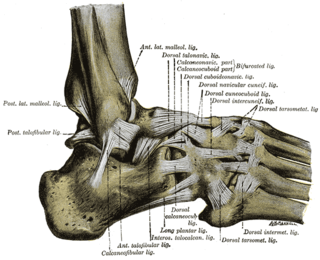
The anterior ligament of the lateral malleolus is a flat, trapezoidal band of fibers, broader below than above, which extends obliquely downward and lateralward between the adjacent margins of the tibia and fibula, on the front aspect of the syndesmosis.

In anatomy, fibrous joints are joints connected by fibrous tissue, consisting mainly of collagen. These are fixed joints where bones are united by a layer of white fibrous tissue of varying thickness. In the skull, the joints between the bones are called sutures. Such immovable joints are also referred to as synarthroses.
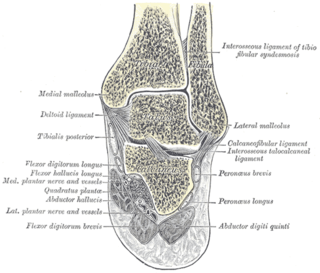
A malleolus is the bony prominence on each side of the human ankle.
A high ankle sprain, also known as a syndesmotic ankle sprain (SAS), is a sprain of the syndesmotic ligaments that connect the tibia and fibula in the lower leg, thereby creating a mortise and tenon joint for the ankle. High ankle sprains are described as high because they are located above the ankle. They comprise approximately 15% of all ankle sprains. Unlike the common lateral ankle sprains, when ligaments around the ankle are injured through an inward twisting, high ankle sprains are caused when the lower leg and foot externally rotates.

The Danis–Weber classification is a method of describing ankle fractures. It has three categories:

A crus fracture is a fracture of the lower legs bones meaning either or both of the tibia and fibula.

A syndesmotic screw is a metal screw designed to replace the syndesmosis of the human body, usually temporarily. If the syndosmosis is torn apart as result of bone fracture, surgeons will sometimes fix the relevant bones together with a syndesmotic screw, temporarily replacing the normal articulation.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:

A Tillaux fracture is a Salter–Harris type III fracture through the anterolateral aspect of the distal tibial epiphysis. It occurs in older adolescents between the ages of 12 and 15 when the medial epiphysis had closed but before the lateral side has done so, due to an avulsion of the anterior inferior tibiofibular ligament, at the opposite end to a Wagstaffe-Le Fort avulsion fracture