| Pancreatoblastoma | |
|---|---|
| Specialty | Oncology |

Pancreatoblastoma is a rare type of pancreatic cancer. [2] It occurs mainly in childhood [3] and has a relatively good prognosis.
| Pancreatoblastoma | |
|---|---|
| Specialty | Oncology |

Pancreatoblastoma is a rare type of pancreatic cancer. [2] It occurs mainly in childhood [3] and has a relatively good prognosis.
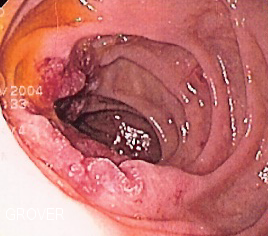
Children with pancreatoblastoma rarely present with early-stage disease, instead, most present with locally advanced or metastatic disease. Common presenting symptoms include abdominal pain, emesis, and jaundice. A multidisciplinary approach including good clinical history, state of the art imaging, and careful pathology is often needed to establish the correct diagnosis. [4]
Resected pancreatoblastomas can be quite large, ranging from 2 centimeters to 20 centimeters in size (1 to 8 inches). They are typically solid, soft masses. Under the microscope, at least two cell types are seen: cells with “acinar” differentiation, and cells forming small “squamoid” nests. The cells with acinar differentiation have some features of the normal acinar cell of the pancreas (the most common cell in the normal pancreas). [5]
| | This section is empty. You can help by adding to it. (March 2018) |
If the tumor is operable, the first line of therapy should be surgical resection. Then, after surgical resection, adjuvant chemotherapy should be given, even in stage I disease. In patients with inoperable disease, chemotherapy alone should be given. [6] A multi-disciplinary approach to the treatment, including surgeons, oncologists, pathologists, radiologists, and radiation oncologists, is often the best approach to managing these patients. [4]
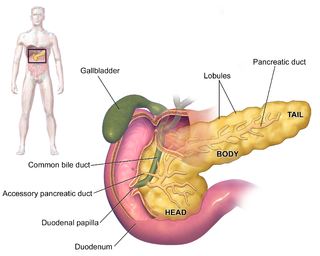
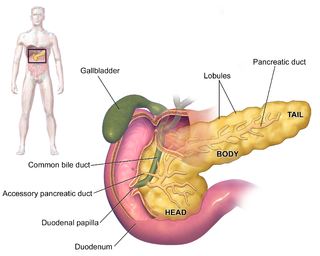
The pancreas is an organ of the digestive system and endocrine system of vertebrates. In humans, it is located in the abdomen behind the stomach and functions as a gland. The pancreas is a mixed or heterocrine gland, i.e., it has both an endocrine and a digestive exocrine function. 99% of the pancreas is exocrine and 1% is endocrine. As an endocrine gland, it functions mostly to regulate blood sugar levels, secreting the hormones insulin, glucagon, somatostatin and pancreatic polypeptide. As a part of the digestive system, it functions as an exocrine gland secreting pancreatic juice into the duodenum through the pancreatic duct. This juice contains bicarbonate, which neutralizes acid entering the duodenum from the stomach; and digestive enzymes, which break down carbohydrates, proteins and fats in food entering the duodenum from the stomach.

Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.

In medicine, a pancreatectomy is the surgical removal of all or part of the pancreas. Several types of pancreatectomy exist, including pancreaticoduodenectomy, distal pancreatectomy, segmental pancreatectomy, and total pancreatectomy. In recent years, the TP-IAT has also gained respectable traction within the medical community. These procedures are used in the management of several conditions involving the pancreas, such as benign pancreatic tumors, pancreatic cancer, and pancreatitis.
Duodenal cancer is a cancer in the first section of the small intestine known as the duodenum. Cancer of the duodenum is relatively rare compared to stomach cancer and colorectal cancer. Its histology is usually adenocarcinoma.

Desmoplastic small-round-cell tumor (DSRCT) is an aggressive and rare cancer that primarily occurs as masses in the abdomen. Other areas affected may include the lymph nodes, the lining of the abdomen, diaphragm, spleen, liver, chest wall, skull, spinal cord, large intestine, small intestine, bladder, brain, lungs, testicles, ovaries, and the pelvis. Reported sites of metastatic spread include the liver, lungs, lymph nodes, brain, skull, and bones. It is characterized by the EWS-WT1 fusion protein.
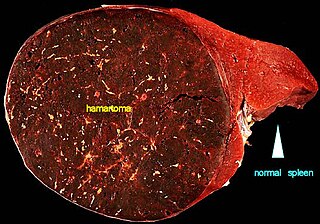
A hamartoma is a mostly benign, local malformation of cells that resembles a neoplasm of local tissue but is usually due to an overgrowth of multiple aberrant cells, with a basis in a systemic genetic condition, rather than a growth descended from a single mutated cell (monoclonality), as would typically define a benign neoplasm/tumor. Despite this, many hamartomas are found to have clonal chromosomal aberrations that are acquired through somatic mutations, and on this basis the term hamartoma is sometimes considered synonymous with neoplasm. Hamartomas are by definition benign, slow-growing or self-limiting, though the underlying condition may still predispose the individual towards malignancies.
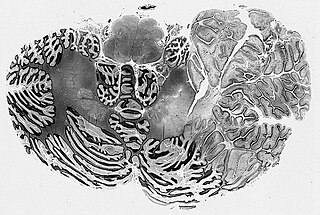
A blastoma is a type of cancer, more common in children, that is caused by malignancies in precursor cells, often called blasts. Examples are nephroblastoma, medulloblastoma, and retinoblastoma. The suffix -blastoma is used to imply a tumor of primitive, incompletely differentiated cells, e.g., chondroblastoma is composed of cells resembling the precursor of chondrocytes.
Ganglioglioma is a rare, slow-growing primary central nervous system (CNS) tumor which most frequently occurs in the temporal lobes of children and young adults

Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lung, and the rest of the body.
Somatostatinomas are a tumor of the delta cells of the endocrine pancreas that produces somatostatin. Increased levels of somatostatin inhibit pancreatic hormones and gastrointestinal hormones. Thus, somatostatinomas are associated with mild diabetes mellitus, steatorrhoea and gallstones, and achlorhydria. Somatostatinomas are commonly found in the head of pancreas. Only ten percent of somatostatinomas are functional tumours [9], and 60–70% of tumours are malignant. Nearly two-thirds of patients with malignant somatostatinomas will present with metastatic disease.
Autoimmune Pancreatitis (AIP) is an increasingly recognized type of chronic pancreatitis that can be difficult to distinguish from pancreatic carcinoma but which responds to treatment with corticosteroids, particularly prednisone. Although autoimmune pancreatitis is quite rare, it constitutes an important clinical problem for both patients and their clinicians: the disease commonly presents itself as a tumorous mass which is diagnostically indistinguishable from pancreatic cancer, a disease that is much more common in addition to being very dangerous. Hence, some patients undergo pancreatic surgery, which is associated to substantial mortality and morbidity, out of the fear by patients and clinicians to undertreat a malignancy. However, surgery is not a good treatment for this condition as AIP responds well to immunosuppressive treatment. There are two categories of AIP: Type 1 and Type 2, each with distinct clinical profiles.

Acinic cell carcinoma is a malignant tumor representing 2% of all salivary tumors. 90% of the time found in the parotid gland, 10% intraorally on buccal mucosa or palate. The disease presents as a slow growing mass, associated with pain or tenderness in 50% of the cases. Often appears pseudoencapsulated.
The Ewing family of tumors (EFTs) is a group of small cell sarcomas including Ewing sarcoma of the bone, extra osseous Ewing tumors, and primitive neuroectodermal tumors. They are rare cancers, usually diagnosed in peoples' twenties. The sarcoma of bone is the most common of the variants. All forms are predisposed to metastasis and have had historically high rates of mortality. The family of tumors shares a common translocation mutation of the EWS gene on chromosome 22 to an ETS-type gene, most commonly the FLI1 gene. EFTs are highly malignant, with 5-year survival for patients with metastatic disease at 20%. The current standard of care includes resection, radiation, and chemotherapy.

Adenocarcinoma of the lung is the most common type of lung cancer, and like other forms of lung cancer, it is characterized by distinct cellular and molecular features. It is classified as one of several non-small cell lung cancers (NSCLC), to distinguish it from small cell lung cancer which has a different behavior and prognosis. Lung adenocarcinoma is further classified into several subtypes and variants. The signs and symptoms of this specific type of lung cancer are similar to other forms of lung cancer, and patients most commonly complain of persistent cough and shortness of breath.
Acinar adenocarcinoma is a histological subtype of gland-forming cancer that is diagnosed when cuboidal and/or columnar shaped malignant cells in the neoplastic tissue form acini and tubules. It is a common form of cancer occurring in the lung and prostate gland.

Ductal cells refer to the epithelial cell lining of the pancreatic duct that deliver enzymes from the acinar cells to the duodenum. They have the essential function of producing bicarbonate-rich (HCO3-) secretion to neutralize stomach acidity. The hormone secretin stimulates ductal cells and is responsible for maintaining the duodenal pH and preventing duodenal injury from acidic chyme. Ductal cells mix their production with acinar cells to make up the pancreatic juice.

Acinar cell carcinoma of the pancreas, also acinar cell carcinoma, is a rare malignant exocrine tumour of the pancreas. It represents 5% of all exocrine tumours of the pancreas, making it the second most common type of pancreatic cancer. It is abbreviated ACC. It typically has a guarded prognosis.
A pancreatic tumor is an abnormal growth in the pancreas. In adults, almost 90% are pancreatic cancer and a few are benign. Pancreatic tumors are rare in children.
Pancreatic mucinous cystic neoplasm (MCN) is a type of cystic lesion that occurs in the pancreas. Amongst individuals undergoing surgical resection of a pancreatic cyst, about 23 percent were mucinous cystic neoplasms. These lesions are benign, though there is a high rate of progression to cancer. As such, surgery should be pursued when feasible. The rate of malignancy present in MCN is about 10 percent. If resection is performed before invasive malignancy develops, prognosis is excellent. The extent of invasion is the single most important prognostic factor in predicting survival.
{{cite journal}}: CS1 maint: multiple names: authors list (link)