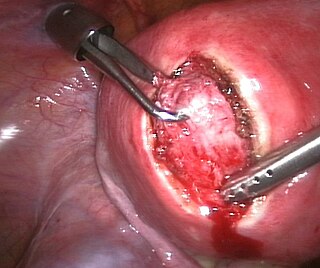
Hysterectomy is the surgical removal of the uterus and cervix. Supracervical hysterectomy refers to removal of the uterus while the cervix is spared. These procedures may also involve removal of the ovaries (oophorectomy), fallopian tubes (salpingectomy), and other surrounding structures. The term “partial” or “total” hysterectomy are lay-terms that incorrectly describe the addition or omission of oophorectomy at the time of hysterectomy. These procedures are usually performed by a gynecologist. Removal of the uterus renders the patient unable to bear children and has surgical risks as well as long-term effects, so the surgery is normally recommended only when other treatment options are not available or have failed. It is the second most commonly performed gynecological surgical procedure, after cesarean section, in the United States. Nearly 68 percent were performed for conditions such as endometriosis, irregular bleeding, and uterine fibroids. It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.

Uterine cancer, also known as womb cancer, includes two types of cancer that develop from the tissues of the uterus. Endometrial cancer forms from the lining of the uterus, and uterine sarcoma forms from the muscles or support tissue of the uterus. Endometrial cancer accounts for approximately 90% of all uterine cancers in the United States. Symptoms of endometrial cancer include changes in vaginal bleeding or pain in the pelvis. Symptoms of uterine sarcoma include unusual vaginal bleeding or a mass in the vagina.
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.
Heavy menstrual bleeding (HMB), previously known as menorrhagia or hematomunia, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).
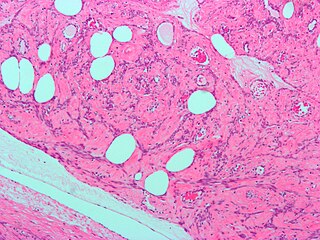
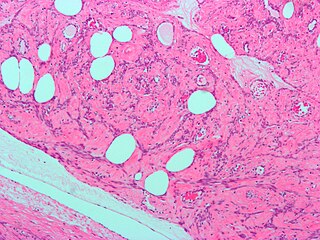
A leiomyoma, also known as a fibroid, is a benign smooth muscle tumor that very rarely becomes cancer (0.1%). They can occur in any organ, but the most common forms occur in the uterus, small bowel, and the esophagus. Polycythemia may occur due to increased erythropoietin production as part of a paraneoplastic syndrome.

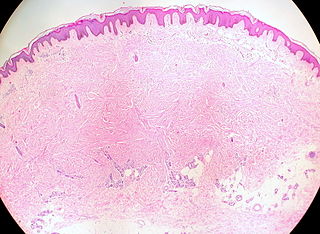
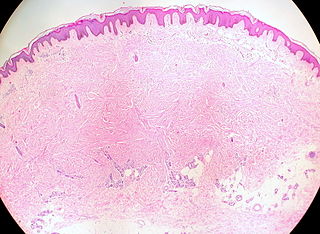
Adenomyosis is a medical condition characterized by the growth of cells that proliferate on the inside of the uterus (endometrium) atypically located among the cells of the uterine wall (myometrium), as a result, thickening of the uterus occurs. As well as being misplaced in patients with this condition, endometrial tissue is completely functional. The tissue thickens, sheds and bleeds during every menstrual cycle.

Vaginal bleeding is any expulsion of blood from the vagina. This bleeding may originate from the uterus, vaginal wall, or cervix. Generally, it is either part of a normal menstrual cycle or is caused by hormonal or other problems of the reproductive system, such as abnormal uterine bleeding.
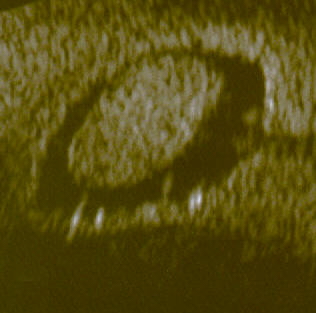
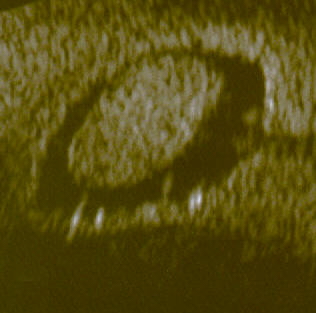
An endometrial polyp or uterine polyp is a mass in the inner lining of the uterus. They may have a large flat base (sessile) or be attached to the uterus by an elongated pedicle (pedunculated). Pedunculated polyps are more common than sessile ones. They range in size from a few millimeters to several centimeters. If pedunculated, they can protrude through the cervix into the vagina. Small blood vessels may be present, particularly in large polyps.

Uterine fibroids, also known as uterine leiomyomas or fibroids, are benign smooth muscle tumors of the uterus, part of the female reproductive system. Some women with fibroids have no symptoms while others may have painful or heavy periods. If large enough, they may push on the bladder, causing a frequent need to urinate. They may also cause pain during penetrative sex or lower back pain. A woman can have one uterine fibroid or many. It is uncommon but possible that fibroids may make it difficult to become pregnant.
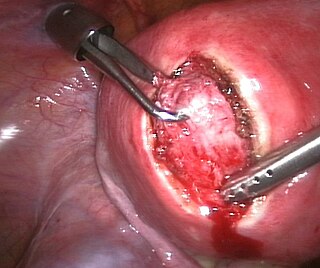
Myomectomy, sometimes also called fibroidectomy, refers to the surgical removal of uterine leiomyomas, also known as fibroids. In contrast to a hysterectomy, the uterus remains preserved and the woman retains her reproductive potential. It still may impact hormonal regulation and the menstrual cycle.

Uterine artery embolization is a procedure in which an interventional radiologist uses a catheter to deliver small particles that block the blood supply to the uterine body. The procedure is primarily done for the treatment of uterine fibroids and adenomyosis. Since uterine fibroids are the most common indication, it is also often referred to as uterine fibroid embolization. Compared to surgical treatment for fibroids such as a hysterectomy, in which a woman's uterus is removed, uterine artery embolization may be beneficial in women who wish to retain their uterus. Other reasons for uterine artery embolization are postpartum hemorrhage and uterine arteriovenous malformations.
Intermenstrual bleeding (IMB) is vaginal bleeding at irregular intervals between expected menstrual periods. It may be associated with bleeding with sexual intercourse.
Adenomyoma is a tumor (-oma) including components derived from glands (adeno-) and muscle (-my-). It is a type of complex and mixed tumor, and several variants have been described in the medical literature. Uterine adenomyoma, the localized form of uterine adenomyosis, is a tumor composed of endometrial gland tissue and smooth muscle in the myometrium. Adenomyomas containing endometrial glands are also found outside of the uterus, most commonly on the uterine adnexa but can also develop at distant sites outside of the pelvis. Gallbladder adenomyoma, the localized form of adenomyomatosis, is a polypoid tumor in the gallbladder composed of hyperplastic mucosal epithelium and muscularis propria.

A menstrual disorder is characterized as any abnormal condition with regards to a woman's menstrual cycle. There are many different types of menstrual disorders that vary with signs and symptoms, including pain during menstruation, heavy bleeding, or absence of menstruation. Normal variations can occur in menstrual patterns but generally menstrual disorders can also include periods that come sooner than 21 days apart, more than 3 months apart, or last more than 10 days in duration. Variations of the menstrual cycle are mainly caused by the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, and early detection and management is required in order to minimize the possibility of complications regarding future reproductive ability.
The uterine sarcomas form a group of malignant tumors that arises from the smooth muscle or connective tissue of the uterus. They can be difficult to detect, as symptoms are common to other uterine conditions and no specific screening test has been developed. This presents an issue for treatment, as the cancer spreads quickly.
Female genital disease is a disorder of the structure or function of the female reproductive system that has a known cause and a distinctive group of symptoms, signs, or anatomical changes. The female reproductive system consists of the ovaries, fallopian tubes, uterus, vagina, and vulva. Female genital diseases can be classified by affected location or by type of disease, such as malformation, inflammation, or infection.

Endometrioma is the presence of tissue similar to, but distinct from, the endometrium in and sometimes on the ovary. It is the most common form of endometriosis. Endometrioma is found in 17–44% patients with endometriosis.

Hereditary leiomyomatosis and renal cell carcinoma (HLRCC) or Reed's syndrome is rare autosomal dominant disorder associated with benign smooth muscle tumors and an increased risk of renal cell carcinoma. It is characterised by multiple cutaneous leiomyomas and, in women, uterine leiomyomas. It predisposes individuals to renal cell cancer, an association denominated hereditary leiomyomatosis and renal cell cancer. It is also associated with increased risk of uterine leiomyosarcoma. The syndrome is caused by a mutation in the fumarate hydratase gene, which leads to an accumulation of fumarate. The inheritance pattern is autosomal dominant and screening can typically begin in childhood.
Elagolix/estradiol/norethisterone acetate, sold under the brand name Oriahnn, is a fixed-dose combination medication used to treat heavy menstrual bleeding associated with uterine leiomyomas (fibroids) in premenopausal women. It contains elagolix, a gonadotropin-releasing hormone (GnRH) receptor antagonist, estradiol, an estrogen, and norethisterone acetate, a progestin. It is taken by mouth. Oriahnn is co-packaged as a combination of elagolix/estradiol/norethisterone acetate capsules with elagolix capsules.
Cutaneous leiomyoma, also known as leiomyoma cutis, or cutaneous leiomyomata, is a benign skin tumor made of smooth muscle cells. There are three different types of cutaneous leiomyomas, genital leiomyomas, angioleiomyomas, and piloleiomyomas. Cutaneous leiomyomas can occur sporadically or as a part of a genetic condition. Cutaneous leiomyomas are diagnosed by histopathology and treated by surgical excision.