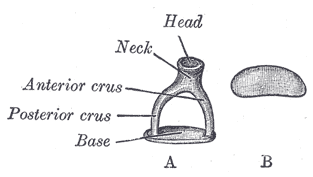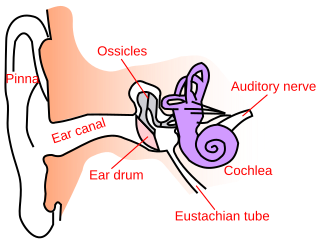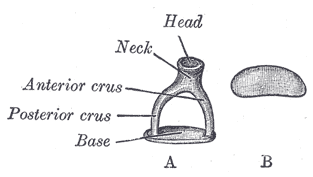
The stapes or stirrup is a bone in the middle ear of humans and other animals which is involved in the conduction of sound vibrations to the inner ear. This bone is connected to the oval window by its annular ligament, which allows the footplate to transmit sound energy through the oval window into the inner ear. The stapes is the smallest and lightest bone in the human body, and is so-called because of its resemblance to a stirrup.

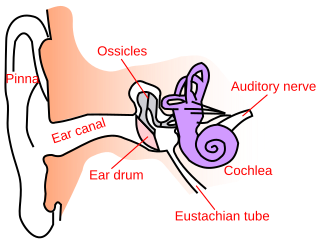
The cochlea is the part of the inner ear involved in hearing. It is a spiral-shaped cavity in the bony labyrinth, in humans making 2.75 turns around its axis, the modiolus. A core component of the cochlea is the organ of Corti, the sensory organ of hearing, which is distributed along the partition separating the fluid chambers in the coiled tapered tube of the cochlea.

The vestibulocochlear nerve or auditory vestibular nerve, also known as the eighth cranial nerve, cranial nerve VIII, or simply CN VIII, is a cranial nerve that transmits sound and equilibrium (balance) information from the inner ear to the brain. Through olivocochlear fibers, it also transmits motor and modulatory information from the superior olivary complex in the brainstem to the cochlea.
Stapedectomy is a surgical procedure in which the stapes bone is removed from the middle ear and replaced with a prosthesis.
Conductive hearing loss (CHL) occurs when there is a problem transferring sound waves anywhere along the pathway through the outer ear, tympanic membrane (eardrum), or middle ear (ossicles). If a conductive hearing loss occurs in conjunction with a sensorineural hearing loss, it is referred to as a mixed hearing loss. Depending upon the severity and nature of the conductive loss, this type of hearing impairment can often be treated with surgical intervention or pharmaceuticals to partially or, in some cases, fully restore hearing acuity to within normal range. However, cases of permanent or chronic conductive hearing loss may require other treatment modalities such as hearing aid devices to improve detection of sound and speech perception.

Sensorineural hearing loss (SNHL) is a type of hearing loss in which the root cause lies in the inner ear or sensory organ or the vestibulocochlear nerve. SNHL accounts for about 90% of reported hearing loss. SNHL is usually permanent and can be mild, moderate, severe, profound, or total. Various other descriptors can be used depending on the shape of the audiogram, such as high frequency, low frequency, U-shaped, notched, peaked, or flat.

The Weber test is a screening test for hearing performed with a tuning fork. It can detect unilateral (one-sided) conductive hearing loss and unilateral sensorineural hearing loss. The test is named after Ernst Heinrich Weber (1795–1878). Conductive hearing ability is mediated by the middle ear composed of the ossicles: the malleus, the incus, and the stapes. Sensorineural hearing ability is mediated by the inner ear composed of the cochlea with its internal basilar membrane and attached cochlear nerve. The outer ear consisting of the pinna, ear canal, and ear drum or tympanic membrane transmits sounds to the middle ear but does not contribute to the conduction or sensorineural hearing ability save for hearing transmissions limited by cerumen impaction.
The Rinne test is used primarily to evaluate loss of hearing in one ear. It compares perception of sounds transmitted by air conduction to those transmitted by bone conduction through the mastoid. Thus, one can quickly screen for the presence of conductive hearing loss.

An audiogram is a graph that shows the audible threshold for standardized frequencies as measured by an audiometer. The Y axis represents intensity measured in decibels (dB) and the X axis represents frequency measured in hertz (Hz). The threshold of hearing is plotted relative to a standardised curve that represents 'normal' hearing, in dB(HL). They are not the same as equal-loudness contours, which are a set of curves representing equal loudness at different levels, as well as at the threshold of hearing, in absolute terms measured in dB SPL.

A bone-anchored hearing aid (BAHA) is a type of hearing aid based on bone conduction. It is primarily suited for people who have conductive hearing losses, unilateral hearing loss, single-sided deafness and people with mixed hearing losses who cannot otherwise wear 'in the ear' or 'behind the ear' hearing aids. They are more expensive than conventional hearing aids, and their placement involves invasive surgery which carries a risk of complications, although when complications do occur, they are usually minor.

The round window is one of the two openings from the middle ear into the inner ear. It is sealed by the secondary tympanic membrane, which vibrates with opposite phase to vibrations entering the inner ear through the oval window. It allows fluid in the cochlea to move, which in turn ensures that hair cells of the basilar membrane will be stimulated and that audition will occur.
Hearing loss with craniofacial syndromes is a common occurrence. Many of these multianomaly disorders involve structural malformations of the outer or middle ear, making a significant hearing loss highly likely.
Electric acoustic stimulation (EAS) is the use of a hearing aid and a cochlear implant technology together in the same ear. EAS is intended for people with high-frequency hearing loss, who can hear low-pitched sounds but not high-pitched ones. The hearing aid acoustically amplifies low-frequency sounds, while the cochlear implant electrically stimulates the middle- and high-frequency sounds. The inner ear then processes the acoustic and electric stimuli simultaneously, to give the patient the perception of sound.
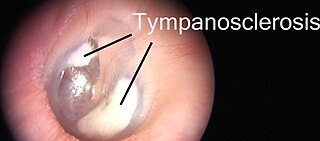
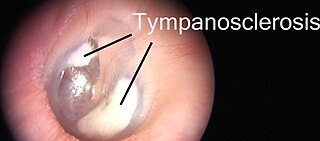
Tympanosclerosis is a condition caused by hyalinization and subsequent calcification of subepithelial connective tissue of the tympanic membrane and middle ear, sometimes resulting in a detrimental effect to hearing.
Bone-conduction auditory brainstem response or BCABR is a type of auditory evoked response that records neural response from EEG with stimulus transmitted through bone conduction.
SoundBite Hearing System is a non-surgical bone conduction prosthetic device that transmits sound via the teeth. It is an alternative to surgical bone conduction prosthetic devices, which require surgical implantation into the skull to conduct sound.
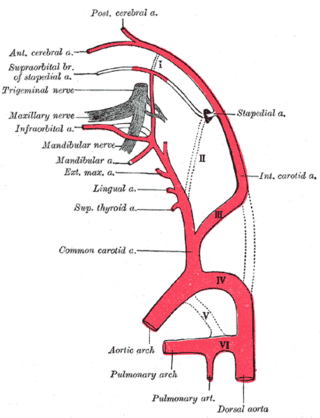
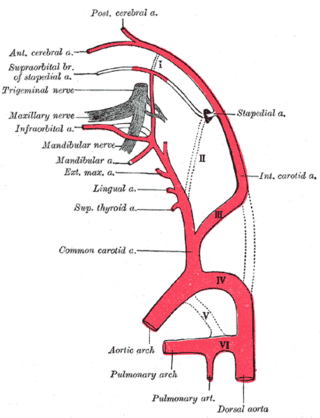
A persistent stapedial artery (PSA) is a rare anomaly in human anatomy where the stapedial branch of posterior auricular artery, or simply stapedial artery, remains within the ear of a fetus after the first ten weeks of pregnancy. Whilst not problematic for the majority of people with the anomaly, it can cause difficulties with hearing.
Causes of hearing loss include ageing, genetics, perinatal problems, loud sounds, and diseases. For some kinds of hearing loss the cause may be classified as of unknown cause.
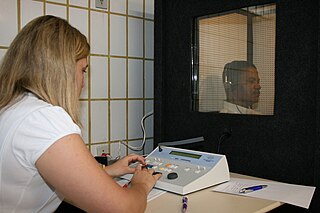
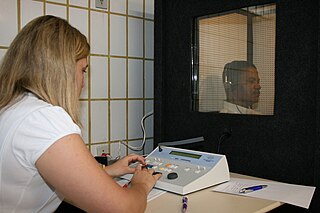
Identification of a hearing loss is usually conducted by a general practitioner medical doctor, otolaryngologist, certified and licensed audiologist, school or industrial audiometrist, or other audiometric technician. Diagnosis of the cause of a hearing loss is carried out by a specialist physician or otorhinolaryngologist.
A middle ear implant is a hearing device that is surgically implanted into the middle ear. They help people with conductive, sensorineural or mixed hearing loss to hear.