Volume 31, Number 1—January 2025
Research
Population-Based Study of Emergence and Spread of Escherichia coli Producing OXA-48–Like Carbapenemases, Israel, 2007–2023
Abstract
Escherichia coli producing OXA-48–like carbapenemases (OXA-EC) is considered a high-risk pathogen spread primarily in the community in low- and middle-income countries and nosocomially in high-income countries. We investigated the emergence and spread of OXA-EC in Israel, a high-income country with strong carbapenemase-directed infection control in healthcare institutions, by conducting a population-based study using data and isolates from the national surveillance system. A total of 3,510 incident cases of OXA-EC occurred during 2007–2023. During 2016–2023, annual cases rose from 41 to 1,524 and nonnosocomial cases rose from 39% to 57%. Sixty-three sequenced isolates belonged to 20 sequence types (STs) and had 3 blaOXA alleles (blaOXA-244, blaOXA-48, and blaOXA-181); 71% were chromosomally encoded, and 29% were plasmid-encoded. Nosocomially and non–nosocomially acquired isolates belonged to the same STs and alleles. Most outbreaks involved multiple STs and could only partially be explained by plasmid dissemination. Measures for confronting OXA-EC might need reconsideration.
Enterobacterales harboring OXA-48–like carbapenemases are notable for their susceptibility to third-generation cephalosporins and low-level resistance to carbapenems (1). Dissemination of blaOXA-48–like occurs by both plasmid transfer and clonal spread (2). Although blaOXA-48–like was initially characterized as exclusively plasmid-borne (1), later reports described chromosomally carried blaOXA-48–like (3). A review published in 2017 reported that blaOXA-48–like was extremely rare in the United States but relatively common in Europe and spreading in the Middle East, Africa, Asia, and South America (4). In high-income countries, most carbapenemase-producing Enterobacterales (CPE) are either nosocomially acquired or imported from CPE-endemic countries, whereas in low- and middle-income countries, community spread is common (5,6). However, a recent study of 1 OXA-48–like Escherichia coli clone (OXA-244–producing sequence type [ST] 38) in Europe concluded that community transmission was its main mode of spread (7).
During 2007–2011, the first 4 cases of OXA-48–like colonization or infection were detected in Israel, all in patients who had been hospitalized in or traveled to Jordan or Georgia (8,9). In 2012, a total of 57 patients were involved in an outbreak of OXA-48–producing Enterobacterales (OXA-PE) in a neonatal intensive care unit (10). Despite a stringent national intervention to limit the spread of CPE in the healthcare system (11), we observed a sharp increase in cases of E. coli producing OXA-48–like carbapenemases (OXA-EC). In 2008, we predicted a scenario of community spread of a plasmidborne carbapenemase in a common human pathogen (12) that appears to be coming true in the form of OXA-EC.
The objective of our study was to describe the spread of OXA-EC in Israel. Specifically, we aimed to determine the incidence of OXA-EC over time and by acquisition source, the proportion of OXA-EC case-patients with no recent history of healthcare exposure (suggesting community transmission), the risk for progression from OXA-EC carriage to bloodstream infection, whether nosocomially acquired and non–nosocomially acquired isolates are related, and whether the OXA-EC epidemic is driven by a single allele, plasmid, or clone. We hypothesized that the increase in OXA-EC incidence stems from community spread of blaOXA-48–like through plasmids on multiple E. coli clones.
Study Design and Setting
The study was a country-level, population-based descriptive study of OXA-EC in Israel during 2007–2023. Israel has conducted active surveillance with mandatory reporting of carbapenem-resistant Enterobacterales (CRE) since 2007. Patients are screened for CPE carriage upon hospital admission if they are transferred from another healthcare facility or were hospitalized in an acute care hospital or long-term care facility in the previous 6 months. Patients are screened during their hospital stay if they had contact with a newly detected CPE carrier or are transferred from a high-risk ward, or as part of routine screening in high-risk wards.
Data Sources
We used data from Israel’s national CRE surveillance system, which records all new cases of CPE detected by screening or clinical culture. In addition, since October 2022, we prospectively investigated new CPE acquisitions that were classified as nonnosocomial to determine the possible source; local infection control staff questioned these patients about contact with the healthcare system in the past year and foreign travel. We used the national surveillance system of bloodstream infections (BSIs) caused by sentinel bacteria to determine the incidence of OXA-EC BSI among patients with OXA-EC first detected by screening.
Definitions
CPE acquisition refers to the first time that CPE with a given carbapenemase was detected in a patient. We classified acquisitions as nosocomial if CPE was detected >48 hours after admission, upon transfer to another healthcare institution, or upon readmission within 30 days. We classified all other acquisitions as nonnosocomial, which includes healthcare-associated cases and imported cases. We defined nosocomial cases as belonging to a ward-level outbreak if >2 cases of nosocomial OXA-EC were detected in the same ward, with <30 days between cases. We defined nosocomial cases as probably hospital-acquired during an outbreak if >2 cases of nosocomial OXA-EC were detected in different wards, with <30 days between cases; we qualified those acquisitions as probable because they might have been cases introduced from the community and detected after the second hospital day.
Laboratory Methods
We conducted CPE screening by rectal swab. We processed specimens according to national guidelines for CRE testing (13). Carbapenemase identification (blaKPC, blaNDM, blaOXA-48–like, and blaVIM) by PCR or lateral flow immunoassay has been mandatory since 2016 for all Enterobacterales growing on screening plates or having a meropenem MIC >0.25 μg/mL. In most laboratories in Israel, screening is performed using mSUPERCARBA (CHROMagar, https://www.chromagar.com), which has high sensitivity (14). Enrichment is not recommended because it delays results needed quickly to guide infection control measures.
We performed additional analyses on 235 OXA-EC isolates collected during 2021–2023 from 34 healthcare institutions. We conducted isolate identification and antibiotic susceptibility testing by using VITEK 2 (bioMérieux, https://www.biomerieux.com) or the disk diffusion method (for imipenem, ertapenem, and ceftazidime/avibactam) based on Clinical and Laboratory Standards Institute breakpoints (15). We determined meropenem MICs by agar dilution. To determine whether the spread of OXA-EC is monoclonal, we performed Fourier-transform infrared spectroscopy (FTIR) by using previously described methods (16). FTIR groups isolates into clusters by phenotype; for E. coli, the clusters are good approximations of clones identified by genotyping (17–19). On the basis of the dendrogram, we selected 63 isolates representing large clusters, small clusters, and singletons; different healthcare facilities; and nosocomial and nonnosocomial acquisitions to undergo whole-genome sequencing (WGS). DNA samples were sequenced using Oxford Nanopore at SNPsaurus (Eugene, OR, USA). We assigned STs to isolates on the basis of the Achtman and Pasteur schemes, and we performed core-genome multilocus sequence typing using PubMLST (https://pubmlst.org). We examined whether nosocomially acquired and non–nosocomially acquired isolates belonged to separate clones or clusters. We also examined whether outbreaks were monoclonal or monocluster.
To understand the role of plasmids in OXA-EC spread, we detected plasmids in sequenced isolates by using PlasmidFinder 2.0.1 (https://cge.food.dtu.dk/services/PlasmidFinder). We performed plasmid visualization by using Proksee (https://proksee.ca). To display the relationship between STs, alleles, and plasmids, we constructed a pan-genome tree by using Roary 3.12.0 (https://bioweb.pasteur.fr/packages/pack@[email protected]), followed by a maximum-likelihood tree built with RAxML 8.2.12 (https://bioweb.pasteur.fr/packages/pack@[email protected]) using the general time-reversible plus gamma model.
Statistical Analysis
We summarized incident cases of OXA-EC occurring during 2007–2023 by using descriptive statistics (percentage or median and interquartile range [IQR]). We plotted an epidemic curve of annual incident cases of Enterobacterales producing OXA-48–like carbapenemases during 2007–2023, stratified by species (E. coli, Klebsiella pneumoniae, and other Enterobacterales). To determine the incidence of OXA-EC over time and by acquisition source, we plotted annual incident OXA-EC cases from 2016 (the start of mandatory carbapenemase testing) to 2023, stratified by acquisition type as defined previously.
We used piecewise linear regression to determine whether the change in cases per 1 million population per year differed among 3 periods (2007–2015, 2016–2021, and 2022–2023). We performed a χ2 test to determine whether the proportion of cases that were nonnosocomial differed between the periods 2016–2021 and 2022–2023. We used data from our prospective investigations of cases detected during October 2022–December 2023 to determine the proportion of OXA-EC cases in persons with no recent history of healthcare exposure. We then calculated the percentage (and exact 95% CI) of patients with OXA-EC first detected by screening who later had OXA-EC BSI. We excluded patients with <2 days of follow-up. We performed those analyses in Stata 14.2 (https://www.stata.com/stata14).
We used the adjusted Wallace coefficient to calculate concordance between: FTIR and MLST, FTIR and OXA-48–like alleles, and MLST and OXA-48–like alleles. We performed the calculations by using an online calculator (20).
Ethics Considerations
The study was approved by the Institutional Review Board at Tel Aviv Sourasky Medical Center. The informed consent requirement was waived for this analysis of routinely collected surveillance data.
Description of Patients
During 2007–2023, a total of 3,510 incident cases of OXA-EC occurred in Israel. The median age of patients was 67 years (IQR 51–78 years), and the median time from acute care hospital admission to detection of nosocomial acquisition was 10 days (IQR 5–18 days) (Table 1).
Trends in OXA-EC Incidence
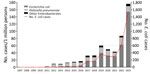
We calculated the annual incidence of E. coli, K. pneumoniae, and other Enterobacterales producing OXA-48–like carbapenemases (Figure 1). No more than 4 annual cases of OXA-EC occurred until 2013; the number rose to 41 in 2016 and to 1,524 in 2023. During 2007–2015, OXA-EC cases per 1 million population increased by 0.7 (95% CI −0.6 to 2.0) per year, but the increase was not significant. Cases per 1 million population increased by 8.1 (95% CI 6.1–10.2) per year during 2016–2021 and by 101.5 (95% CI 85.6–117.5) per year during 2022–2023. The change in slope between the later 2 periods was significant (93.4 [95% CI 76.4–110.4]). In contrast, cases of K. pneumoniae producing OXA-48–like carbapenemases per 1 million population increased by only 1.0 (95% CI 0.1–1.9) per year during 2016–2021 and decreased nonsignificantly by 0.7 (95% CI −7.5 to 6.1) per year during 2022–2023. In both periods, the annual rate of cases of other Enterobacterales producing OXA-48–like carbapenemases did not change significantly. Cases of all species producing OXA-48–like carbapenemases declined during 2020–2021, the years of the SARS-CoV-2 pandemic.
Place of Acquisition
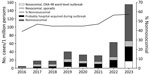
We calculated the incidence of OXA-EC cases by type of acquisition and by year since 2016 (Figure 2). The percentage of cases that were nonnosocomial was significantly higher during 2022–2023 than during 2016–2021 (57.0% vs. 45.3%; p<0.001). Most nosocomial cases (83.0%) were acquired in acute care hospitals (Table 1).
We analyzed the results of the prospective investigation of sources of OXA-EC acquisition conducted during October 2022–December 2023 (Table 2; Appendix Table 1). Of 1,750 cases, 1,000 (57.1%) were nonnosocomial. Of those, 518 (51.8%) occurred in patients who had contact with the healthcare system in Israel during the previous year, 53 (5.3%) cases were imported, and 429 cases (24.5% of all cases) were classified as community-acquired.
OXA-EC BSI
Throughout the study period, 41 cases of BSI caused by OXA-EC occurred. Among the 3,356 patients with OXA-EC first detected by screening, 16 later had OXA-EC BSI (0.5% [95% CI 0.3%–0.8%]).
Susceptibility of OXA-EC
We further characterized 235 OXA-EC isolates stored at the reference laboratory; they comprised 10% of new cases detected during 2021–2023. A total of 220 (93.6%) isolates were susceptible to meropenem, 44.0% to ceftazidime, 43.2% to ceftriaxone, and 96.2% to ceftazidime/avibactam (Appendix Table 2). Of the meropenem-susceptible isolates, 170 (77.3%) had an MIC <0.25.
Clonal Analysis of OXA-EC
A dendrogram generated by FTIR (Appendix Figure 1) shows that OXA-EC isolates belong to multiple clusters. The 235 isolates formed 59 singletons, 25 small clusters (2–5 isolates), and 7 large clusters (>6 isolates). Large clusters accounted for 106 (45.1%) isolates. We selected 63 representative isolates for WGS. They comprised 20 STs based on the Achtman scheme and 14 STs based on the Pasteur scheme.
Association between Clusters/STs and Acquisition Site
Of 19 FTIR clusters containing >3 isolates, 15 contained both nosocomial and non-nosocomial isolates (including those classified as community-acquired). Likewise, we found both nosocomial and nonnosocomial isolates in all 5 of the Achtman STs that included isolates from >3 unique patients.
Clonality of Outbreaks
The dendrogram includes 100 isolates from patients with nosocomial OXA-EC acquired during a ward-level or hospital-wide outbreak. No outbreaks for which we tested >1 isolate were monocluster or monoclonal. For example, the 22 isolates from an outbreak at hospital E during January–August 2023 comprised 1 dominant cluster (no. 371) and 5 singletons (and >3 STs). Conversely, clusters and STs were not hospital-specific; the largest cluster (no. 381) contained 28 isolates acquired in 6 hospitals and outside the hospital.
Allele Distribution
WGS revealed that OXA-EC belonged to 3 blaOXA-48–like alleles: blaOXA-244 (n = 36, 57.1%), blaOXA-48 (n = 17, 27.0%), and blaOXA-181 (n = 10, 15.9%). All 3 alleles were present in both nosocomial and nonnosocomial isolates (including isolates classified as community-acquired).
Concordance between FTIR and WGS Results
Concordance between FTIR clusters and Achtman STs was high (0.98 [95% CI 0.96–1.00]); all isolates in each FTIR cluster (except for cluster no. 368) belonged to a single ST. We also observed high concordance between FTIR clusters and alleles (0.97 [95% CI 0.94–1.0]), whereas concordance between Achtman STs and alleles was low (0.42 [95% CI 0.29–0.55]). Because ST typing indicates more distant evolutionary origins than FTIR, the difference in concordance suggests that the introduction of the blaOXA-48–like alleles into E. coli populations is a relatively recent event. This conclusion is also supported by the finding that no allele was associated with only 1 ST.
Role of Plasmids
We identified and visualized 3 different plasmids carrying blaOXA-48–like (Appendix Figures 2–4). The plasmids were found in 29% of the sequenced isolates. The transfer of plasmids could only partially explain the nonclonal spread of OXA-EC. In all 10 OXA-181–producing isolates, blaOXA-181 was carried on the composite plasmid ColKP3-IncX3. Among the 17 OXA-48–producing isolates, in 3 blaOXA-48 was carried on the plasmid IncL(pOXA-48) and in 5 blaOXA-48 was carried on the composite plasmid IncFII(pRSB107)–IncFIA-IncFIB(AP001918); 9 isolates had no plasmid. All isolates encoding the blaOXA-244 allele had no plasmid.
Dissemination of Alleles and Plasmids within STs
We examined the relationships among STs, alleles, and plasmids of the sequenced isolates (Figure 3). Alleles and plasmids were scattered among different and distant STs. Only a fraction of allele distribution among STs correlated with plasmid distribution among STs. These results indicate independent outbreaks of the 3 blaOXA-48–like alleles, involving multiple STs, each with a different molecular mode of spread: blaOXA-181 is transmitted through a single plasmid between different STs, blaOXA-48 spreads by 2 plasmids and by the expansion of ST38 carrying blaOXA-48 on the chromosome, and blaOXA-244 is chromosomally encoded and found on 9 STs, suggesting multiple introductions of this gene into the E. coli population.
We studied the epidemiology and molecular epidemiology of OXA-EC in Israel during 2007–2023. The incidence of OXA-EC colonization or infection has risen sharply. As we hypothesized, the proportion of cases that are non-nosocomial has risen, comprising more than half of cases during 2022–2023; approximately one quarter were community-acquired. However, the number of hospital-acquired cases also rose, particularly in 2023, probably because of inadequate detection and isolation of imported cases. The risk for OXA-EC bacteremia among OXA-EC carriers was low (0.5%). Most OXA-EC isolates (93.6%) were susceptible to meropenem, and 44.0% were susceptible to ceftazidime. The spread of OXA-EC represents parallel dissemination of 3 different blaOXA-48–like alleles occurring in multiple clusters and STs. Nosocomial OXA-EC outbreaks often included >1 clone, which might indicate either detection of unrelated OXA-EC carriers who might have introduced the strain from the community or transmission of the blaOXA-like gene between clones through mobile elements. Contrary to our hypothesis that ongoing plasmid spread of blaOXA-48–like to multiple E. coli clones caused the rise in incidence, we found that blaOXA-48–like was not carried on plasmids in more than two thirds of sequenced isolates. Reports on the proportion of OXA-PE that is community-acquired are scarce (21,22). A scoping review of CPE in the community noted that most studies do not distinguish between infection or colonization that is community-acquired versus community-onset (which might be healthcare associated) (23). A survey from 2020–2021 examining OXA-244–producing E. coli ST38 in Europe determined that community transmission was the main mode of spread; evidence included the high proportion of isolates from outpatient urine samples and the geographic dispersion of cases within countries (7). The authors suggested that transmission might be foodborne.
As in previous studies (3,24), we found that blaOXA-244 is encoded chromosomally, indicating that it was introduced into the E. coli population on multiple occasions, integrated into the chromosome, and lost its ability to mobilize to other strains. Thus, in Israel, the spread of OXA-244–producing E. coli is by parallel expansion of multiple clones. In contrast, blaOXA-181 was encoded on a plasmid, and its dissemination was driven by plasmid spread and by the expansion of clones carrying the plasmid. blaOXA-48 had a mixed mode of spread; 2 different plasmids carried this allele and were found in 47% of the isolates, whereas the allele was chromosomally encoded in 53% of the isolates.
We found that nosocomial outbreaks were polyclonal and that not all polyclonal spread was plasmid driven. Several possible explanations exist for these polyclonal, non–plasmid-driven outbreaks. First, nondominant clusters within an outbreak might indicate cases that were present but not detected upon admission. Second, as the result of introduction and diversification of existing clones, multiple clusters/STs might be spreading simultaneously in a single institution, as researchers have described in multidrug-resistant Acinetobacter baumannii (25). Third, mobile genetic elements other than plasmids might transfer blaOXA-48–like between clones.
The rising incidence of OXA-EC indicates that the measures that contained Israel’s outbreak of K. pneumoniae carbapenemase–producing K. pneumoniae (screening, isolation, cohorting, and staff cohorting) (11) are not sufficient to control OXA-EC. Possible reasons for this failure are, first, unidentified community sources of OXA-EC, such as livestock, wildlife, and fresh vegetables (26,27); such sources are unaffected by hospital-based infection control measures. Second, community acquisition of OXA-EC means that the healthcare-focused criteria for screening at hospital admission are inadequate, leading to in-hospital spread by carriers who are undetected and not isolated. Third, when screening occurs, the low MICs of most OXA-EC might curtail their detection as CPE, and thus carriers are not isolated. Fourth, reservoirs in the hospital environment, such as mattresses and sinks, might be a source of OXA-PE spread (26,27). Fifth, although plasmids were not the dominant mode of transmission of sequenced OXA-EC in our study, traditional CPE control measures are less effective in limiting plasmid-mediated nosocomial transmission than clonal spread (28).
Our findings raise policy questions regarding OXA-EC control efforts in hospitals. Most OXA-EC are carbapenemase-producing but not carbapenem-resistant. Given the low risk for severe infection among carriers, the availability of treatment options, and substantial spread outside of the hospital, the question is whether targeting of infection control efforts toward OXA-EC should be stopped. The benefit would be a sharp decrease in the number of patients requiring epidemiologic investigation and isolation. The risk is that nosocomial transmission will probably accelerate, creating a growing reservoir of carriers that would eventually translate into a higher number of clinical infections. Moreover, although we found high in vitro susceptibility to meropenem and moderate-to-high in vitro susceptibility to third-generation cephalosporins and aminoglycosides, a gap exists between in vitro and in vivo success; some studies have reported high rates of clinical failure and death among patients with severe infections caused by OXA-PE (7,29).
One limitation of our study is that PCR for blaOXA-48–like was not universally used before 2016, probably leading to undercounting of cases in earlier years. In addition, the indications for CPE screening in the hospital might be too narrow to identify community-acquired OXA-EC cases, also leading to undercounting in later years. Moreover, nonnosocomial cases might have been misclassified as nosocomial because they were not detected at hospital admission. Further, FTIR and WGS were performed only on a fraction of isolates; additional clusters, STs, alleles, and plasmids might have gone undetected.
In conclusion, the emergence and rise of OXA-EC is concerning and challenges well-established strategies of CRE control. Infection control policymakers should consider the option of demoting OXA-EC from its status as a high-risk pathogen. However, any loosening of restrictions on OXA-EC carriers must be accompanied by monitoring for unintended consequences.
Dr. Temkin is a senior epidemiologist in the National Institute for Antibiotic Resistance and Infection Control in Tel Aviv, Israel. She conducts research and surveillance related to hospital-acquired infections and antibiotic resistance.
Acknowledgments
Members of the CPE Working Group: Tal Brosh-Nissimov (Assuta Ashdod University Hospital and Faculty of Health Sciences, Ben Gurion University), Nadav Sorek (Assuta Ashdod University Hospital); Haim Ben Zvi, Rita Chervets, Nataliya Halel Wolf, Orli Nisimov, Bina Rubinovitch (Rabin Medical Center, Beilinson Hospital); Tamar Boumard, Evgeniya Gofaizen, Bracha Mendelson, Alona Paz (Bnei Zion Medical Center); Mirit Hershman-Sarafov (Bnei Zion Medical Center and Rappaport Faculty of Medicine, Technion); Marina Feldman, Ola Salah (Carmel Medical Center); Ronza Najjar-Debbiny (Carmel Medical Center and Rappaport Faculty of Medicine, Technion); Iris Avraham, Merav Strauss (Emek Medical Center); Bibiana Chazan (Emek Medical Center and Rappaport Faculty of Medicine, Technion); Tal Bendahan, Ayelet Favor, Ilana Gross, Kamy Harpaz, Jana Hen, Miriam Ottolenghi, Eleonora Radvogin, Nechamat Reichman, Naama Ronen, Nehama Shilo, Shady Zahran (Hadassah Medical Center); Yonatan Oster (Hadassah Medical Center and Faculty of Medicine, Hebrew University); Rina Fedorowsky, Rebecca Yerushalmi (Hasharon Hospital); Tamar Gottesman (Hasharon Hospital and Faculty of Medical and Health Sciences, Tel Aviv University); Orna Ben Natan, Muhammed Ganayem, Aliza Vaknin (Hillel Yaffe Medical Center); Regev Cohen (Hillel Yaffe Medical Centre and Rappaport Faculty of Medicine, Technion); Rita Bardenstein, Pnina Ciobotaro, Chen Uliel (Kaplan Medical Center); Marina Afraimov, Daniell Atiya (Laniado Hospital); Jonathan Lellouche (Laniado Hospital and Adelson School of Medicine, Ariel University); Bat Sheva Kloyzner (Mayanei Hayeshua Medical Center); Haia Arielly, Ofra Benisty, (Meir Medical Center); Pnina Shitrit (Meir Medical Center and Faculty of Medical and Health Sciences, Tel Aviv University); David Schwartz (National Institute for Antibiotic Resistance and Infection Control); Amir Nutman, Vered Schechner (National Institute for Antibiotic Resistance and Infection Control and Faculty of Medical and Health Sciences, Tel Aviv University); Worood Aboalhega, Tamar Alon, Ibraheem Firan, Moran Hamo, Elena Lomansov, Sigal Mendelsohn, Dina Pollak, Moran Szwarcwort Cohen, Jalal Tarabeia (Rambam Health Care Campus); Meirav Mor (Schneider Children's Medical Center and Faculty of Medical and Health Sciences, Tel Aviv University); Sigalit Rozenfeld (Schneider Children's Medical Center); Samar Abu Ghosh, Batcheva Ezagui (Shaare Zedek Medical Center); Marc Assous, Shmuel Benenson (Shaare Zedek Medical Center and Faculty of Medicine, Hebrew University); Olga Bondar, Lili Goldshtein, Diana Nestor (Shamir Medical Center); Jalal Abu Hanna, Margarita Berbi, Oryan Henig, Anna Medovy, Sarit Stepansky (Tel Aviv Sourasky Medical Center); Maya Azrad (Tzafon Medical Center); Hiba Zayyad (Tzafon Medical Center and Azrieli Faculty of Medicine, Bar-Ilan University); Debby Ben-David (Wolfson Medical Center and Faculty of Medical and Health Sciences, Tel Aviv University); and Yael Cohen (Wolfson Medical Center)
Genomes of the 63 sequenced isolates were deposited in the BioProject database under accession nos. PRJNA1028854 and PRJNA1144649.
No external funding was received for this work. Y.C. has received grants and personal fees from Enlivex Therapeutics, MSD, Pfizer, Roche, Qpex Pharmaceuticals, and Spero Therapeutics. T.B.-N. has received consulting fees and payments or honoraria from AstraZeneca, MSD, GSK, Gilead, and Medison. Y.O. has received grants from Gilead and BioFence.
References
- Poirel L, Héritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48:15–22. DOIPubMedGoogle Scholar
- Pitout JDD, Peirano G, Kock MM, Strydom K-A, Matsumura Y. The global ascendency of OXA-48-type carbapenemases. Clin Microbiol Rev. 2019;33:e00102–19. DOIPubMedGoogle Scholar
- Emeraud C, Girlich D, Bonnin RA, Jousset AB, Naas T, Dortet L. Emergence and polyclonal dissemination of OXA-244–producing Escherichia coli, France. Emerg Infect Dis. 2021;27:1206–10. DOIPubMedGoogle Scholar
- van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae. Virulence. 2017;8:460–9. DOIPubMedGoogle Scholar
- van Duin D, Paterson DL. Multidrug-resistant bacteria in the community: an update. Infect Dis Clin North Am. 2020;34:709–22. DOIPubMedGoogle Scholar
- Nicolas-Chanoine M-H, Vigan M, Laouénan C, Robert J; “E-carb Study Group”. Risk factors for carbapenem-resistant Enterobacteriaceae infections: a French case-control-control study. Eur J Clin Microbiol Infect Dis. 2019;38:383–93. DOIPubMedGoogle Scholar
- European Centre for Disease Prevention and Control. Increase in OXA-244–producing Escherichia coli in the European Union/European Economic Area and the UK since 2013–first update. 2021 [cited 2024 Apr 28]. https://www.ecdc.europa.eu/sites/default/files/documents/OXA-244-producing-E-coli-in-EU-EEA-since-2013-first-update.pdf
- Goren MG, Chmelnitsky I, Carmeli Y, Navon-Venezia S. Plasmid-encoded OXA-48 carbapenemase in Escherichia coli from Israel. J Antimicrob Chemother. 2011;66:672–3. DOIPubMedGoogle Scholar
- Adler A, Shklyar M, Schwaber MJ, Navon-Venezia S, Dhaher Y, Edgar R, et al. Introduction of OXA-48-producing Enterobacteriaceae to Israeli hospitals by medical tourism. J Antimicrob Chemother. 2011;66:2763–6. DOIPubMedGoogle Scholar
- Adler A, Solter E, Masarwa S, Miller-Roll T, Abu-Libdeh B, Khammash H, et al. Epidemiological and microbiological characteristics of an outbreak caused by OXA-48-producing Enterobacteriaceae in a neonatal intensive care unit in Jerusalem, Israel. J Clin Microbiol. 2013;51:2926–30. DOIPubMedGoogle Scholar
- Schwaber MJ, Lev B, Israeli A, Solter E, Smollan G, Rubinovitch B, et al.; Israel Carbapenem-Resistant Enterobacteriaceae Working Group. Containment of a country-wide outbreak of carbapenem-resistant Klebsiella pneumoniae in Israeli hospitals via a nationally implemented intervention. Clin Infect Dis. 2011;52:848–55. DOIPubMedGoogle Scholar
- Schwaber MJ, Carmeli Y. Carbapenem-resistant Enterobacteriaceae: a potential threat. JAMA. 2008;300:2911–3. DOIPubMedGoogle Scholar
- Solter E, Adler A, Rubinovitch B, Temkin E, Schwartz D, Ben-David D, et al. Israeli national policy for carbapenem-resistant Enterobacteriaceae screening, carrier isolation and discontinuation of isolation. Infect Control Hosp Epidemiol. 2018;39:85–9. DOIPubMedGoogle Scholar
- Garcia-Quintanilla M, Poirel L, Nordmann P. CHROMagar mSuperCARBA and RAPIDEC® Carba NP test for detection of carbapenemase-producing Enterobacteriaceae. Diagn Microbiol Infect Dis. 2018;90:77–80. DOIPubMedGoogle Scholar
- Clinical and Laboratory Standard Institute. Performance standards for antimicrobial susceptibility testing, 33rd edition (M100). Wayne (PA): The Institute; 2023.
- Rakovitsky N, Frenk S, Kon H, Schwartz D, Temkin E, Solter E, et al. Fourier transform infrared spectroscopy is a new option for outbreak investigation: a retrospective analysis of an extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae outbreak in a neonatal intensive care unit. J Clin Microbiol. 2020;58:e00098–20. DOIPubMedGoogle Scholar
- Teng ASJ, Habermehl PE, van Houdt R, de Jong MD, van Mansfeld R, Matamoros SPF, et al. Comparison of fast Fourier transform infrared spectroscopy biotyping with whole genome sequencing-based genotyping in common nosocomial pathogens. Anal Bioanal Chem. 2022;414:7179–89. DOIPubMedGoogle Scholar
- Uribe G, Salipante SJ, Curtis L, Lieberman JA, Kurosawa K, Cookson BT, et al. Evaluation of Fourier transform-infrared spectroscopy (FT-IR) as a control measure for nosocomial outbreak investigations. J Clin Microbiol. 2023;61:
e0034723 . DOIPubMedGoogle Scholar - Kon H, Lurie-Weinberger MN, Lugassy C, Chen D, Schechner V, Schwaber MJ, et al. Use of Fourier-transform infrared spectroscopy for real-time outbreak investigation of OXA-48-producing Escherichia coli. J Antimicrob Chemother. 2024;79:349–53. DOIPubMedGoogle Scholar
- Molecular Microbiology and Infection Unit. Comparing partitions. 2011 [cited 2024 May 1]. http://www.comparingpartitions.info
- Bulens SN, Reses HE, Ansari UA, Grass JE, Carmon C, Albrecht V, et al. Carbapenem-Resistant enterobacterales in individuals with and without health care risk factors -Emerging infections program, United States, 2012-2015. Am J Infect Control. 2023;51:70–7. DOIPubMedGoogle Scholar
- Shrestha R, Luterbach CL, Dai W, Komarow L, Earley M, Weston G, et al.; MDRO Investigators. Characteristics of community-acquired carbapenem-resistant Enterobacterales. J Antimicrob Chemother. 2022;77:2763–71. DOIPubMedGoogle Scholar
- Kelly AM, Mathema B, Larson EL. Carbapenem-resistant Enterobacteriaceae in the community: a scoping review. Int J Antimicrob Agents. 2017;50:127–34. DOIPubMedGoogle Scholar
- Hoyos-Mallecot Y, Naas T, Bonnin RA, Patino R, Glaser P, Fortineau N, et al. OXA-244–producing Escherichia coli isolates, a challenge for clinical microbiology laboratories. Antimicrob Agents Chemother. 2017;61:e00818–17. DOIPubMedGoogle Scholar
- Marchaim D, Navon-Venezia S, Leavitt A, Chmelnitsky I, Schwaber MJ, Carmeli Y. Molecular and epidemiologic study of polyclonal outbreaks of multidrug-resistant Acinetobacter baumannii infection in an Israeli hospital. Infect Control Hosp Epidemiol. 2007;28:945–50. DOIPubMedGoogle Scholar
- Boyd SE, Holmes A, Peck R, Livermore DM, Hope W. OXA-48-like β-lactamases: global epidemiology, treatment options, and development pipeline. Antimicrob Agents Chemother. 2022;66:
e0021622 . DOIPubMedGoogle Scholar - Mairi A, Pantel A, Sotto A, Lavigne J-P, Touati A. OXA-48-like carbapenemases producing Enterobacteriaceae in different niches. Eur J Clin Microbiol Infect Dis. 2018;37:587–604. DOIPubMedGoogle Scholar
- Marimuthu K, Venkatachalam I, Koh V, Harbarth S, Perencevich E, Cherng BPZ, et al.; Carbapenemase-Producing Enterobacteriaceae in Singapore (CaPES) Study Group. Whole genome sequencing reveals hidden transmission of carbapenemase-producing Enterobacterales. Nat Commun. 2022;13:3052. DOIPubMedGoogle Scholar
- Kidd JM, Livermore DM, Nicolau DP. The difficulties of identifying and treating Enterobacterales with OXA-48-like carbapenemases. Clin Microbiol Infect. 2020;26:401–3. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: December 10, 2024
1Members of the working group are listed at the end of this article.
Table of Contents – Volume 31, Number 1—January 2025
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Elizabeth Temkin, National Institute for Antibiotic Resistance and Infection Control, 6 Weizmann St, Tel Aviv, 6423906, Israel
Top