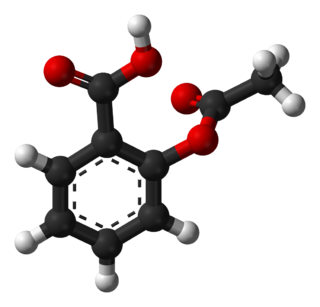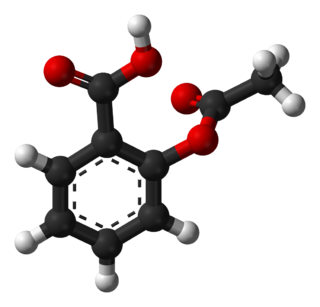
Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and inflammation, and as an antithrombotic. Specific inflammatory conditions that aspirin is used to treat include Kawasaki disease, pericarditis, and rheumatic fever.

Non-steroidal anti-inflammatory drugs (NSAID) are members of a therapeutic drug class which reduces pain, decreases inflammation, decreases fever, and prevents blood clots. Side effects depend on the specific drug, its dose and duration of use, but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.

Prostaglandins (PG) are a group of physiologically active lipid compounds called eicosanoids that have diverse hormone-like effects in animals. Prostaglandins have been found in almost every tissue in humans and other animals. They are derived enzymatically from the fatty acid arachidonic acid. Every prostaglandin contains 20 carbon atoms, including a 5-carbon ring. They are a subclass of eicosanoids and of the prostanoid class of fatty acid derivatives.

Arachidonic acid is a polyunsaturated omega−6 fatty acid 20:4(ω−6), or 20:4(5,8,11,14). If its precursors or diet contains linoleic acid it is formed by biosynthesis and can be deposited in animal fats. It is a precursor in the formation of leukotrienes, prostaglandins, and thromboxanes.

Cyclooxygenase (COX), officially known as prostaglandin-endoperoxide synthase (PTGS), is an enzyme that is responsible for biosynthesis of prostanoids, including thromboxane and prostaglandins such as prostacyclin, from arachidonic acid. A member of the animal-type heme peroxidase family, it is also known as prostaglandin G/H synthase. The specific reaction catalyzed is the conversion from arachidonic acid to prostaglandin H2 via a short-living prostaglandin G2 intermediate.
Cyclooxygenase-2 inhibitors, also known as coxibs, are a type of nonsteroidal anti-inflammatory drug (NSAID) that directly target cyclooxygenase-2 (COX-2), an enzyme responsible for inflammation and pain. Targeting selectivity for COX-2 reduces the risk of peptic ulceration and is the main feature of celecoxib, rofecoxib, and other members of this drug class.

Prostacyclin (also called prostaglandin I2 or PGI2) is a prostaglandin member of the eicosanoid family of lipid molecules. It inhibits platelet activation and is also an effective vasodilator.

Thromboxane is a member of the family of lipids known as eicosanoids. The two major thromboxanes are thromboxane A2 and thromboxane B2. The distinguishing feature of thromboxanes is a 6-membered ether-containing ring.

Indometacin, also known as indomethacin, is a nonsteroidal anti-inflammatory drug (NSAID) commonly used as a prescription medication to reduce fever, pain, stiffness, and swelling from inflammation. It works by inhibiting the production of prostaglandins, endogenous signaling molecules known to cause these symptoms. It does this by inhibiting cyclooxygenase, an enzyme that catalyzes the production of prostaglandins.

The thromboxane receptor (TP) also known as the prostanoid TP receptor is a protein that in humans is encoded by the TBXA2R gene, The thromboxane receptor is one among the five classes of prostanoid receptors and was the first eicosanoid receptor cloned. The TP receptor derives its name from its preferred endogenous ligand thromboxane A2.
A prostaglandin antagonist is a hormone antagonist acting upon one or more prostaglandins, a subclass of eicosanoid compounds which function as signaling molecules in numerous types of animal tissues.

Thromboxane A2 (TXA2) is a type of thromboxane that is produced by activated platelets during hemostasis and has prothrombotic properties: it stimulates activation of new platelets as well as increases platelet aggregation. This is achieved by activating the thromboxane receptor, which results in platelet-shape change, inside-out activation of integrins, and degranulation. Circulating fibrinogen binds these receptors on adjacent platelets, further strengthening the clot. TXA2 is also a known vasoconstrictor and is especially important during tissue injury and inflammation. It is also regarded as responsible for Prinzmetal's angina.

Prostaglandin H2 (PGH2), or prostaglandin H2 (PGH2), is a type of prostaglandin and a precursor for many other biologically significant molecules. It is synthesized from arachidonic acid in a reaction catalyzed by a cyclooxygenase enzyme. The conversion from arachidonic acid to prostaglandin H2 is a two-step process. First, COX-1 catalyzes the addition of two free oxygens to form the 1,2-dioxane bridge and a peroxide functional group to form prostaglandin G2 (PGG2). Second, COX-2 reduces the peroxide functional group to a secondary alcohol, forming prostaglandin H2. Other peroxidases like hydroquinone have been observed to reduce PGG2 to PGH2. PGH2 is unstable at room temperature, with a half life of 90–100 seconds, so it is often converted into a different prostaglandin.

Cyclooxygenase-2 (COX-2), also known as prostaglandin-endoperoxide synthase 2 (HUGO PTGS2), is an enzyme that in humans is encoded by the PTGS2 gene. In humans it is one of three cyclooxygenases. It is involved in the conversion of arachidonic acid to prostaglandin H2, an important precursor of prostacyclin, which is expressed in inflammation.

Cyclooxygenase 1 (COX-1), also known as prostaglandin-endoperoxide synthase 1, is an enzyme that in humans is encoded by the PTGS1 gene. In humans it is one of two cyclooxygenases.
Cyclooxygenases are enzymes that take part in a complex biosynthetic cascade that results in the conversion of polyunsaturated fatty acids to prostaglandins and thromboxane(s). Their main role is to catalyze the transformation of arachidonic acid into the intermediate prostaglandin H2, which is the precursor of a variety of prostanoids with diverse and potent biological actions. Cyclooxygenases have two main isoforms that are called COX-1 and COX-2. COX-1 is responsible for the synthesis of prostaglandin and thromboxane in many types of cells, including the gastro-intestinal tract and blood platelets. COX-2 plays a major role in prostaglandin biosynthesis in inflammatory cells and in the central nervous system. Prostaglandin synthesis in these sites is a key factor in the development of inflammation and hyperalgesia. COX-2 inhibitors have analgesic and anti-inflammatory activity by blocking the transformation of arachidonic acid into prostaglandin H2 selectively.
Thromboregulation is the series of mechanisms in how a primary clot is regulated. These mechanisms include, competitive inhibition or negative feedback. It includes primary hemostasis, which is the process of how blood platelets adhere to the endothelium of an injured blood vessel. Platelet aggregation is fundamental to repair vascular damage and the initiation of the blood thrombus formation. The elimination of clots is also part of thromboregulation. Failure in platelet clot regulation may cause hemorrhage or thrombosis. Substances called thromboregulators control every part of these events.

12-Hydroxyheptadecatrienoic acid (also termed 12-HHT, 12(S)-hydroxyheptadeca-5Z,8E,10E-trienoic acid, or 12(S)-HHTrE) is a 17 carbon metabolite of the 20 carbon polyunsaturated fatty acid, arachidonic acid. 12-HHT is less ambiguously termed 12-(S)-hydroxy-5Z,8E,10E-heptadecatrienoic acid to indicate the S stereoisomerism of its 12-hydroxyl residue and the Z, E, and E cis–trans isomerism of its three double bonds. 12-HHT was discovered and structurally defined in 1973 by Paulina Wlodawer, Bengt Samuelsson, and Mats Hamberg. It was identified as a product of arachidonic acid metabolism made by microsomes isolated from sheep seminal vesicle glands and by intact human platelets. 12-HHT was for many years thought to be merely a biologically inactive byproduct of prostaglandin synthesis. More recent studies, however, have attached potentially important activity to it.
Prostaglandin inhibitors are drugs that inhibit the synthesis of prostaglandin in human body. There are various types of prostaglandins responsible for different physiological reactions such as maintaining the blood flow in stomach and kidney, regulating the contraction of involuntary muscles and blood vessels, and act as a mediator of inflammation and pain. Cyclooxygenase (COX) and Phospholipase A2 are the major enzymes involved in prostaglandin production, and they are the drug targets for prostaglandin inhibitors. There are mainly 2 classes of prostaglandin inhibitors, namely non- steroidal anti- inflammatory drugs (NSAIDs) and glucocorticoids. In the following sections, the medical uses, side effects, contraindications, toxicity and the pharmacology of these prostaglandin inhibitors will be discussed.

Lysine acetylsalicylate, also known as aspirin DL-lysine or lysine aspirin, is a more soluble form of acetylsalicylic acid (aspirin). As with aspirin itself, it is a nonsteroidal anti-inflammatory drug (NSAID) with analgesic, anti-inflammatory, antithrombotic and antipyretic properties. It is composed of the ammonium form of the amino acid lysine paired with the conjugate base of aspirin.