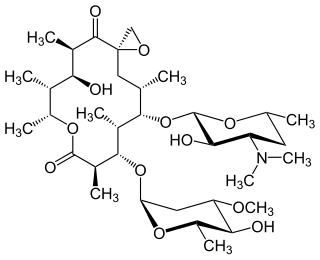
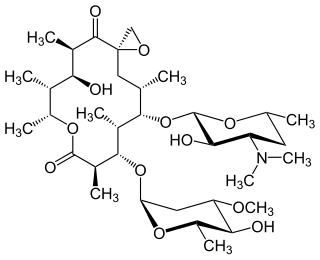
Erythromycin is an antibiotic used for the treatment of a number of bacterial infections. This includes respiratory tract infections, skin infections, chlamydia infections, pelvic inflammatory disease, and syphilis. It may also be used during pregnancy to prevent Group B streptococcal infection in the newborn, and to improve delayed stomach emptying. It can be given intravenously and by mouth. An eye ointment is routinely recommended after delivery to prevent eye infections in the newborn.

Clarithromycin, sold under the brand name Biaxin among others, is an antibiotic used to treat various bacterial infections. This includes strep throat, pneumonia, skin infections, H. pylori infection, and Lyme disease, among others. Clarithromycin can be taken by mouth as a tablet or liquid or can be infused intravenously.

Drug resistance is the reduction in effectiveness of a medication such as an antimicrobial or an antineoplastic in treating a disease or condition. The term is used in the context of resistance that pathogens or cancers have "acquired", that is, resistance has evolved. Antimicrobial resistance and antineoplastic resistance challenge clinical care and drive research. When an organism is resistant to more than one drug, it is said to be multidrug-resistant.
This is the timeline of modern antimicrobial (anti-infective) therapy. The years show when a given drug was released onto the pharmaceutical market. This is not a timeline of the development of the antibiotics themselves.

Clindamycin is a lincosamide antibiotic medication used for the treatment of a number of bacterial infections, including osteomyelitis (bone) or joint infections, pelvic inflammatory disease, strep throat, pneumonia, acute otitis media, and endocarditis. It can also be used to treat acne, and some cases of methicillin-resistant Staphylococcus aureus (MRSA). In combination with quinine, it can be used to treat malaria. It is available by mouth, by injection into a vein, and as a cream or a gel to be applied to the skin or in the vagina.

Azithromycin, sold under the brand names Zithromax and Azasite, is an antibiotic medication used for the treatment of a number of bacterial infections. This includes middle ear infections, strep throat, pneumonia, traveler's diarrhea, and certain other intestinal infections. Along with other medications, it may also be used for malaria. It is administered by mouth, into a vein, or into the eye.
Ketolides are antibiotics belonging to the macrolide group. Ketolides are derived from erythromycin by substituting the cladinose sugar with a keto-group and attaching a cyclic carbamate group in the lactone ring. These modifications give ketolides much broader spectrum than other macrolides. Moreover, ketolides are effective against macrolide-resistant bacteria, due to their ability to bind at two sites at the bacterial ribosome as well as having a structural modification that makes them poor substrates for efflux-pump mediated resistance.

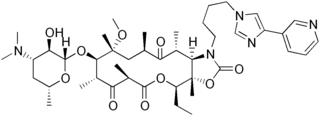
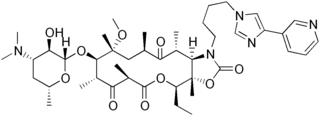
Telithromycin is the first ketolide antibiotic to enter clinical use and is sold under the brand name of Ketek. It is used to treat community acquired pneumonia of mild to moderate severity. After significant safety concerns, the US Food and Drug Administration sharply curtailed the approved uses of the drug in early 2007.

Cytochrome P450 3A4 is an important enzyme in the body, mainly found in the liver and in the intestine, which in humans is encoded by CYP3A4 gene. It oxidizes small foreign organic molecules (xenobiotics), such as toxins or drugs, so that they can be removed from the body. It is highly homologous to CYP3A5, another important CYP3A enzyme.

Clavulanic acid is a β-lactam drug that functions as a mechanism-based β-lactamase inhibitor. While not effective by itself as an antibiotic, when combined with penicillin-group antibiotics, it can overcome antibiotic resistance in bacteria that secrete β-lactamase, which otherwise inactivates most penicillins.

Lincosamides are a class of antibiotics, which include lincomycin, clindamycin, and pirlimycin.

Azalides such as azithromycin are a class of macrolide antibiotics that were originally manufactured in response to the poor acid stability exhibited by original macrolides (erythromycin). Following the clinical overuse of macrolides and azalides, ketolides have been developed to combat surfacing macrolide-azalide resistance among streptococci species. Azalides have several advantages over erythromycin such as more potent gram negative antimicrobial activity, acid stability, and side effect tolerability. Although there are few drug interactions with azithromycin, it weakly inhibits the CYP3A4 enzyme.
Oleandomycin is a macrolide antibiotic. It is synthesized from strains of Streptomyces antibioticus. It is weaker than erythromycin.

Beta-lactamases are a family of enzymes involved in bacterial resistance to beta-lactam antibiotics. In bacterial resistance to beta-lactam antibiotics, the bacteria have beta-lactamase which degrade the beta-lactam rings, rendering the antibiotic ineffective. However, with beta-lactamase inhibitors, these enzymes on the bacteria are inhibited, thus allowing the antibiotic to take effect. Strategies for combating this form of resistance have included the development of new beta-lactam antibiotics that are more resistant to cleavage and the development of the class of enzyme inhibitors called beta-lactamase inhibitors. Although β-lactamase inhibitors have little antibiotic activity of their own, they prevent bacterial degradation of beta-lactam antibiotics and thus extend the range of bacteria the drugs are effective against.

Desosamine is a 3-(dimethylamino)-3,4,6-trideoxyhexose found in certain macrolide antibiotics such as the commonly prescribed erythromycin, azithromycin, clarithroymcin, methymycin, narbomycin, oleandomycin, picromycin and roxithromycin. As the name suggests, these macrolide antibiotics contain a macrolide or lactone ring and they are attached to the ring Desosamine which is crucial for bactericidal activity. The biological action of the desosamine-based macrolide antibiotics is to inhibit the bacterial ribosomal protein synthesis. These antibiotics which contain Desosamine are widely used to cure bacterial-causing infections in human respiratory system, skin, muscle tissues, and urethra.

Diffuse panbronchiolitis (DPB) is an inflammatory lung disease of unknown cause. It is a severe, progressive form of bronchiolitis, an inflammatory condition of the bronchioles. The term diffuse signifies that lesions appear throughout both lungs, while panbronchiolitis refers to inflammation found in all layers of the respiratory bronchioles. DPB causes severe inflammation and nodule-like lesions of terminal bronchioles, chronic sinusitis, and intense coughing with large amounts of sputum production.
Streptogramin A is a group of antibiotics within the larger family of antibiotics known as streptogramins. They are synthesized by the bacteria Streptomyces virginiae. The streptogramin family of antibiotics consists of two distinct groups: group A antibiotics contain a 23-membered unsaturated ring with lactone and peptide bonds while group B antibiotics are depsipeptides. While structurally different, these two groups of antibiotics act synergistically, providing greater antibiotic activity than the combined activity of the separate components. These antibiotics have until recently been commercially manufactured as feed additives in agriculture, although today there is increased interest in their ability to combat antibiotic-resistant bacteria, particularly vancomycin-resistant bacteria.

Solithromycin is a ketolide antibiotic undergoing clinical development for the treatment of community-acquired pneumonia and other infections.

Neisseria gonorrhoeae, the bacterium that causes the sexually transmitted infection gonorrhea, has developed antibiotic resistance to many antibiotics. The bacteria was first identified in 1879.
Anti-ulcer agents are medications or supplements used to cure the damage of mucosal layer on organs to prevent the damage from further extending to deeper regions to cause complications.