Related Research Articles

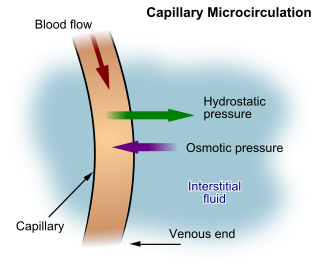
Bleeding, hemorrhage, haemorrhage or blood loss is blood escaping from the circulatory system from damaged blood vessels. Bleeding can occur internally, or externally either through a natural opening such as the mouth, nose, ear, urethra, vagina or anus, or through a puncture in the skin. Hypovolemia is a massive decrease in blood volume, and death by excessive loss of blood is referred to as exsanguination. Typically, a healthy person can endure a loss of 10–15% of the total blood volume without serious medical difficulties. The stopping or controlling of bleeding is called hemostasis and is an important part of both first aid and surgery.
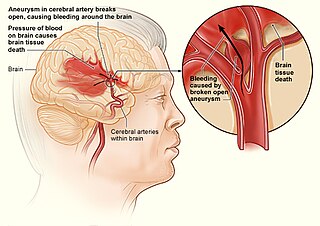
Internal bleeding is a loss of blood from a blood vessel that collects inside the body, and is not usually visible from the outside. It can be a serious medical emergency but the extent of severity depends on bleeding rate and location of the bleeding. Severe internal bleeding into the chest, abdomen, pelvis, or thighs can cause hemorrhagic shock or death if proper medical treatment is not received quickly. Internal bleeding is a medical emergency and should be treated immediately by medical professionals.

Major trauma is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, blunt and penetrating, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility may be necessary to prevent loss of life or limb. The initial assessment is critical, and involves a physical evaluation and also may include the use of imaging tools to determine the types of injuries accurately and to formulate a course of treatment.
Hypovolemic shock is a form of shock caused by severe hypovolemia. It can be caused by severe dehydration or blood loss. Hypovolemic shock is a medical emergency; if left untreated, the insufficient blood flow can cause damage to organs, leading to multiple organ failure.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, and sports-related injuries, and are notably common among the elderly who experience falls.

Focused assessment with sonography in trauma is a rapid bedside ultrasound examination performed by surgeons, emergency physicians, and paramedics as a screening test for blood around the heart or abdominal organs (hemoperitoneum) after trauma. There is also the extended FAST (eFAST) which includes some additional ultrasound views to assess for pneumothorax.
Hemoperitoneum is the presence of blood in the peritoneal cavity. The blood accumulates in the space between the inner lining of the abdominal wall and the internal abdominal organs. Hemoperitoneum is generally classified as a surgical emergency; in most cases, urgent laparotomy is needed to identify and control the source of the bleeding. In selected cases, careful observation may be permissible. The abdominal cavity is highly distensible and may easily hold greater than five liters of blood, or more than the entire circulating blood volume for an average-sized individual. Therefore, large-scale or rapid blood loss into the abdomen will reliably induce hemorrhagic shock and, if untreated, may rapidly lead to death.

Blunt splenic trauma occurs when a significant impact to the spleen from some outside source damages or ruptures the spleen. Treatment varies depending on severity, but often consists of embolism or splenectomy.

A gunshot wound (GSW) is a penetrating injury caused by a projectile from a gun. Damage may include bleeding, bone fractures, organ damage, wound infection, loss of the ability to move part of the body, and in severe cases, death. Damage depends on the part of the body hit, the path the bullet follows through the body, and the type and speed of the bullet. Long-term complications can include bowel obstruction, failure to thrive, neurogenic bladder and paralysis, recurrent cardiorespiratory distress and pneumothorax, hypoxic brain injury leading to early dementia, amputations, chronic pain and pain with light touch (hyperalgesia), deep venous thrombosis with pulmonary embolus, limb swelling and debility, and lead poisoning.

Penetrating trauma is an open wound injury that occurs when an object pierces the skin and enters a tissue of the body, creating a deep but relatively narrow entry wound. In contrast, a blunt or non-penetrating trauma may have some deep damage, but the overlying skin is not necessarily broken and the wound is still closed to the outside environment. The penetrating object may remain in the tissues, come back out the path it entered, or pass through the full thickness of the tissues and exit from another area.
Abdominal compartment syndrome (ACS) occurs when the abdomen becomes subject to increased pressure reaching past the point of intra-abdominal hypertension (IAH). ACS is present when intra-abdominal pressure rises and is sustained at > 20 mmHg and there is new organ dysfunction or failure. ACS is classified into three groups: Primary, secondary and recurrent ACS. It is not a disease and as such it occurs in conjunction with many disease processes, either due to the primary illness or in association with treatment interventions. Specific cause of abdominal compartment syndrome is not known, although some causes can be sepsis and severe abdominal trauma. Increasing pressure reduces blood flow to abdominal organs and impairs pulmonary, cardiovascular, renal, and gastro-intestinal (GI) function, causing obstructive shock, multiple organ dysfunction syndrome and death.
An exploratory laparotomy is a general surgical operation where the abdomen is opened and the abdominal organs are examined for injury or disease. It is the standard of care in various blunt and penetrating trauma situations in which there may be life-threatening internal injuries. It is also used in certain diagnostic situations, in which the operation is undertaken in search of a unifying cause for multiple signs and symptoms of disease, and in the staging of some cancers.
The Wittmann Patch is a temporary abdominal fascia prosthesis for the planned open abdomen to ease the management of cases where the abdomen cannot be closed due to abdominal compartment syndrome or because multiple further operations are planned. It consists of a sterile hook and a sterile loop sheet made from propylene and nylon.

Peter Meong Rhee is an American surgeon, medical professor, and military veteran. During his 24 years in the United States Navy, Rhee served as a battlefield casualty physician in Afghanistan and Iraq.
Trauma surgery is a surgical specialty that utilizes both operative and non-operative management to treat traumatic injuries, typically in an acute setting. Trauma surgeons generally complete residency training in general surgery and often fellowship training in trauma or surgical critical care. The trauma surgeon is responsible for initially resuscitating and stabilizing and later evaluating and managing the patient. The attending trauma surgeon also leads the trauma team, which typically includes nurses and support staff, as well as resident physicians in teaching hospitals.

A stab wound is a specific form of penetrating trauma to the skin that results from a knife or a similar pointed object. While stab wounds are typically known to be caused by knives, they can also occur from a variety of implements, including broken bottles and ice picks. Most stabbings occur because of intentional violence or through self-infliction. The treatment is dependent on many different variables such as the anatomical location and the severity of the injury. Even though stab wounds are inflicted at a much greater rate than gunshot wounds, they account for less than 10% of all penetrating trauma deaths.

A liver injury, also known as liver laceration, is some form of trauma sustained to the liver. This can occur through either a blunt force such as a car accident, or a penetrating foreign object such as a knife. Liver injuries constitute 5% of all traumas, making it the most common abdominal injury. Generally nonoperative management and observation is all that is required for a full recovery.
Early appropriate care (EAC) is a system in orthopaedic trauma surgery aiming to identify serious major trauma patients and treat the most time-critical injuries without adding to their physiological burden.
Endovascular and hybrid trauma and bleeding management is a new and rapidly evolving concept within medical healthcare and endovascular resuscitation. It involves early multidisciplinary evaluation and management of hemodynamically unstable patients with traumatic injuries as well as being a bridge to definitive treatment. It has recently been shown that the EVTM concept may also be applied to non-traumatic hemodynamically unstable patients.

Resuscitative endovascular balloon occlusion of the aorta (REBOA) is a minimally invasive procedure performed during resuscitation of critically injured trauma patients. Originally developed as a less invasive alternative to emergency thoracotomy with aortic cross clamping, REBOA is performed to gain rapid control of non-compressible truncal or junctional hemorrhage. REBOA is performed first by achieving access to the common femoral artery (CFA) and advancing a catheter within the aorta. Upon successful catheter placement, an occluding balloon may be inflated either within the descending thoracic aorta or infrarenal abdominal aorta. REBOA stanches downstream hemorrhage and improves cardiac index, cerebral perfusion, and coronary perfusion. Although REBOA does not eliminate the need for definitive hemorrhage control, it may serve as a temporizing measure during initial resuscitation. Despite the benefits of REBOA, there are significant local and systemic ischemic risks. Establishing standardized REBOA procedural indications and mitigating the risk of ischemic injury are topics of ongoing investigation. Although this technique has been successfully deployed in adult patients, it has not yet been studied in children.
References
- ↑ Jaunoo SS, Harji DP (April 2009). "Damage control surgery". International Journal of Surgery (London, England). 7 (2): 110–3. doi: 10.1016/j.ijsu.2009.01.008 . PMID 19303379.
- ↑ Fries, C. A.; Midwinter, M. J. (2010). "Trauma resuscitation and damage control surgery". Surgery (Oxford). 28 (11): 563. doi:10.1016/j.mpsur.2010.08.002.
- ↑ Garth Meckler; Cline, David; Cydulka, Rita K.; Thomas, Stephen R.; Dan Handel (2012). Tintinalli's Emergency Medicine Manual 7/E. McGraw-Hill Professional. ISBN 978-0-07-178184-8.
- 1 2 3 4 5 Duchesne, Juan C.; McSwain, Norman E.; Cotton, Bryan A.; Hunt, John P.; Dellavolpe, Jeff; Lafaro, Kelly; Marr, Alan B.; Gonzalez, Earnest A.; Phelan, Herb A.; Bilski, Tracy; Greiffenstein, Patrick; Barbeau, James M.; Rennie, Kelly V.; Baker, Christopher C.; Brohi, Karim; Jenkins, Donald H.; Rotondo, Michael (October 2010). "Damage Control Resuscitation: The New Face of Damage Control". The Journal of Trauma: Injury, Infection, and Critical Care. 69 (4): 976–990. doi:10.1097/TA.0b013e3181f2abc9. PMID 20938283. S2CID 10787586.
- 1 2 Rotondo, Michael F.; Schwab, C. William; McGonigal, Michael D.; Phillips, Gordon R.; Fruchterman, Todd M.; Kauder, Donald R.; Latenser, Barbara A.; Angood, Peter A. (September 1993). "Damage Control". The Journal of Trauma: Injury, Infection, and Critical Care. 35 (3): 375–383. doi: 10.1097/00005373-199309000-00008 . PMID 8371295.
- 1 2 Johnson, Jon W.; Gracias, Vicente H.; Schwab, C. William; Reilly, Patrick M.; Kauder, Donald R.; Shapiro, Michael B.; Dabrowski, G. Paul; Rotondo, Michael F. (August 2001). "Evolution in Damage Control for Exsanguinating Penetrating Abdominal Injury". The Journal of Trauma: Injury, Infection, and Critical Care. 51 (2): 261–271. doi:10.1097/00005373-200108000-00007. PMID 11493783.
- 1 2 Pringle, J Hogarth (October 1908). "V. Notes on the Arrest of Hepatic Hemorrhage Due to Trauma". Annals of Surgery. 48 (4): 541–9. doi:10.1097/00000658-190810000-00005. PMC 1406963 . PMID 17862242.
- ↑ Reilly, Patrick M.; Rotondo, Michael F.; Carpenter, Jeffrey P.; Sherr, Scott A.; Schwab, C. William (October 1995). "Temporary Vascular Continuity during Damage Control". The Journal of Trauma: Injury, Infection, and Critical Care. 39 (4): 757–760. doi:10.1097/00005373-199510000-00028. PMID 7473971.
- 1 2 Hoey, BA; Schwab, CW (2002). "Damage control surgery". Scandinavian Journal of Surgery. 91 (1): 92–103. doi:10.1177/145749690209100115. PMID 12075844. S2CID 73006797.
- ↑ Brown, Laura R.; Rentea, Rebecca M. (2024), "Temporary Abdominal Closure Techniques", StatPearls, Treasure Island, FL: StatPearls Publishing, PMID 33232048 , retrieved 2024-06-28
- ↑ Ouellet, Jean-Francois; Ball, Chad G. (September 2011). "Recurrent abdominal compartment syndrome induced by high negative pressure abdominal closure dressing". The Journal of Trauma. 71 (3): 785–786. doi:10.1097/TA.0b013e31822bbde5. ISSN 1529-8809. PMID 21909013.
- ↑ Miller, Richard S.; Morris, John A.; Diaz, Jose J.; Herring, Michael B.; May, Addison K. (December 2005). "Complications after 344 Damage-Control Open Celiotomies". The Journal of Trauma: Injury, Infection, and Critical Care. 59 (6): 1365–1374. doi:10.1097/01.ta.0000196004.49422.af. PMID 16394910.
- ↑ Bickell, William H.; Wall, Matthew J.; Pepe, Paul E.; Martin, R. Russell; Ginger, Victoria F.; Allen, Mary K.; Mattox, Kenneth L. (27 October 1994). "Immediate versus Delayed Fluid Resuscitation for Hypotensive Patients with Penetrating Torso Injuries". New England Journal of Medicine. 331 (17): 1105–1109. doi: 10.1056/NEJM199410273311701 . PMID 7935634.
- 1 2 Holcomb JB, Pati S. Optimal trauma resuscitation with plasma as the primary resuscitative fluid: the surgeon's perspective. Hematology Am Soc Hematol Educ Program. 2013; 656-9.
- 1 2 Holcomb, John B.; del Junco, Deborah J.; Fox, Erin E.; Wade, Charles E.; Cohen, Mitchell J.; Schreiber, Martin A.; Alarcon, Louis H.; Bai, Yu; Brasel, Karen J.; Bulger, Eileen M.; Cotton, Bryan A.; Matijevic, Nena; Muskat, Peter; Myers, John G.; Phelan, Herb A.; White, Christopher E.; Zhang, Jiajie; Rahbar, Mohammad H.; PROMMTT Study Group, for the (1 February 2013). "The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) Study". JAMA Surgery. 148 (2): 127–36. doi:10.1001/2013.jamasurg.387. PMC 3740072 . PMID 23560283.
- 1 2 Callcut, Rachael A.; Cotton, Bryan A.; Muskat, Peter; Fox, Erin E.; Wade, Charles E.; Holcomb, John B.; Schreiber, Martin A.; Rahbar, Mohammad H.; Cohen, Mitchell J.; Knudson, M. Margaret; Brasel, Karen J.; Bulger, Eileen M.; del Junco, Deborah J.; Myers, John G.; Alarcon, Louis H.; Robinson, Bryce R.H. (January 2013). "Defining when to initiate massive transfusion". Journal of Trauma and Acute Care Surgery. 74 (1): 59–68. doi:10.1097/TA.0b013e3182788b34. PMC 3771339 . PMID 23271078.
- 1 2 Nunez, Timothy C.; Young, Pampee P.; Holcomb, John B.; Cotton, Bryan A. (June 2010). "Creation, Implementation, and Maturation of a Massive Transfusion Protocol for the Exsanguinating Trauma Patient". The Journal of Trauma: Injury, Infection, and Critical Care. 68 (6): 1498–1505. doi:10.1097/TA.0b013e3181d3cc25. PMC 3136378 . PMID 20539192.
- ↑ Brohi 2008
- ↑ Lucas, Charles E; Ledgerwood, Anna M (June 1976). "Prospective evaluation of hemostatic techniques for liver injuries". The Journal of Trauma. 16 (6): 442–51. doi:10.1097/00005373-197606000-00003. PMID 778397.
- 1 2 Feliciano, DV; Mattox, KL; Jordan GL, Jr (April 1981). "Intra-abdominal packing for control of hepatic hemorrhage: a reappraisal". The Journal of Trauma. 21 (4): 285–90. doi: 10.1097/00005373-198104000-00005 . PMID 7012380.
- 1 2 3 Stone HH, Strom PR, Mullins RJ (May 1983). "Management of the major coagulopathy with onset during laparotomy". Annals of Surgery. 197 (5): 532–5. doi:10.1097/00000658-198305000-00005. PMC 1353025 . PMID 6847272.
- ↑ Rotondo MF, Schwab CW, McGonigal MD, et al. (September 1993). "'Damage control': an approach for improved survival in exsanguinating penetrating abdominal injury". The Journal of Trauma. 35 (3): 375–82, discussion 382–3. doi: 10.1097/00005373-199309000-00008 . PMID 8371295.
- ↑ Rotondo, Michael F.; Zonies, David H. (August 1997). "The damage control sequence and underlying logic". Surgical Clinics of North America. 77 (4): 761–777. doi: 10.1016/S0039-6109(05)70582-X . PMID 9291979.
- ↑ Moore, Ernest E.; Burch, Jon M.; Franciose, Reginald J.; Offner, Patrick J.; Biffl, Walter L. (14 March 2014). "Staged Physiologic Restoration and Damage Control Surgery". World Journal of Surgery. 22 (12): 1184–1191. doi: 10.1007/s002689900542 . PMID 9841741. S2CID 10040060.
- ↑ Hirshberg, Asher; Wall, Matthew J.; Mattox, Kenneth L. (September 1994). "Planned Reoperation for Trauma". The Journal of Trauma: Injury, Infection, and Critical Care. 37 (3): 365–369. doi:10.1097/00005373-199409000-00005. PMID 8083894.
- ↑ Barker, Donald E.; Green, John M.; Maxwell, Robert A.; Smith, Philip W.; Mejia, Vicente A.; Dart, Benjamin W.; Cofer, Joseph B.; Roe, S. Michael; Burns, R. Phillip (May 2007). "Experience with Vacuum-Pack Temporary Abdominal Wound Closure in 258 Trauma and General and Vascular Surgical Patients". Journal of the American College of Surgeons. 204 (5): 784–792. doi:10.1016/j.jamcollsurg.2006.12.039. PMID 17481484.
- ↑ Finlay, I. G.; Edwards, T. J.; Lambert, A. W. (January 2004). "Damage control laparotomy". British Journal of Surgery. 91 (1): 83–85. doi: 10.1002/bjs.4434 . PMID 14716799. S2CID 6509240.
- ↑ Ekeh, Akpofure Peter; McCarthy, Mary C.; Woods, Randy J.; Walusimbi, Mbaga; Saxe, Jonathan M.; Patterson, Lisa A. (March 2006). "Delayed closure of ventral abdominal hernias after severe trauma". The American Journal of Surgery. 191 (3): 391–395. doi:10.1016/j.amjsurg.2005.10.045. PMID 16490553.