Clinical death is the medical term for cessation of blood circulation and breathing, the two criteria necessary to sustain the lives of human beings and of many other organisms. [1] It occurs when the heart stops beating in a regular rhythm, a condition called cardiac arrest. The term is also sometimes used in resuscitation research.
Stopped blood circulation has historically proven irreversible in most cases. Prior to the invention of cardiopulmonary resuscitation (CPR), defibrillation, epinephrine injection, and other treatments in the 20th century, the absence of blood circulation (and vital functions related to blood circulation) was historically considered the official definition of death. With the advent of these strategies, cardiac arrest came to be called clinical death rather than simply death, to reflect the possibility of post-arrest resuscitation.
At the onset of clinical death, consciousness is lost within several seconds, and in dogs, measurable brain activity has been measured to stop within 20 to 40 seconds. [2] Irregular gasping may occur during this early time period, and is sometimes mistaken by rescuers as a sign that CPR is not necessary. [3] During clinical death, all tissues and organs in the body steadily accumulate a type of injury called ischemic injury.
Most tissues and organs of the body can survive clinical death for considerable periods. Blood circulation can be stopped in the entire body below the heart for at least 30 minutes, with injury to the spinal cord being a limiting factor. [4] Detached limbs may be successfully reattached after 6 hours of no blood circulation at warm temperatures. Bone, tendon, and skin can survive as long as 8 to 12 hours. [5]
The brain, however, appears to accumulate ischemic injury faster than any other organ. Without special treatment after circulation is restarted, full recovery of the brain after more than 3 minutes of clinical death at normal body temperature is rare. [6] [7] Usually brain damage or later brain death results after longer intervals of clinical death even if the heart is restarted and blood circulation is successfully restored. Brain injury is therefore the chief limiting factor for recovery from clinical death.
Although loss of function is almost immediate, there is no specific duration of clinical death at which the non-functioning brain clearly dies. The most vulnerable cells in the brain, CA1 neurons of the hippocampus, are fatally injured by as little as 10 minutes without oxygen. However, the injured cells do not actually die until hours after resuscitation. [8] This delayed death can be prevented in vitro by a simple drug treatment even after 20 minutes without oxygen. [9] In other areas of the brain, viable human neurons have been recovered and grown in culture hours after clinical death. [10] Brain failure after clinical death is now known to be due to a complex series of processes called reperfusion injury that occur after blood circulation has been restored, especially processes that interfere with blood circulation during the recovery period. [11] Control of these processes is the subject of ongoing research.
In 1990, the laboratory of resuscitation pioneer Peter Safar discovered that reducing body temperature by three degrees Celsius after restarting blood circulation could double the time window of recovery from clinical death without brain damage from 5 minutes to 10 minutes. This induced hypothermia technique is beginning to be used in emergency medicine. [12] [13] The combination of mildly reducing body temperature, reducing blood cell concentration, and increasing blood pressure after resuscitation was found especially effective –allowing for recovery of dogs after 12 minutes of clinical death at normal body temperature with practically no brain injury. [14] [15] The addition of a drug treatment protocol has been reported to allow recovery of dogs after 16 minutes of clinical death at normal body temperature with no lasting brain injury. [16] Cooling treatment alone has permitted recovery after 17 minutes of clinical death at normal temperature, but with brain injury. [17]
Under laboratory conditions at normal body temperature, the longest period of clinical death of a cat (after complete circulatory arrest) survived with eventual return of brain function is one hour. [18] [19]
Reduced body temperature, or therapeutic hypothermia, during clinical death slows the rate of injury accumulation, and extends the time period during which clinical death can be survived. The decrease in the rate of injury can be approximated by the Q10 rule, which states that the rate of biochemical reactions decreases by a factor of two for every 10 °C reduction in temperature. As a result, humans can sometimes survive periods of clinical death exceeding one hour at temperatures below 20 °C. [20] The prognosis is improved if clinical death is caused by hypothermia rather than occurring prior to it; in 1999, 29-year-old Swedish woman Anna Bågenholm spent 80 minutes trapped in ice and survived with a near full recovery from a 13.7 °C core body temperature. It is said in emergency medicine that "nobody is dead until they are warm and dead." [21] In animal studies, up to three hours of clinical death can be survived at temperatures near 0 °C. [22] [23]
The purpose of cardiopulmonary resuscitation (CPR) during cardiac arrest is ideally reversal of the clinically dead state by restoration of blood circulation and breathing. However, there is great variation in the effectiveness of CPR for this purpose. Blood pressure is very low during manual CPR, [24] resulting in only a ten-minute average extension of survival. [25] Yet there are cases of patients regaining consciousness during CPR while still in full cardiac arrest. [26] In absence of cerebral function monitoring or frank return to consciousness, the neurological status of patients undergoing CPR is intrinsically uncertain. It is somewhere between the state of clinical death and a normal functioning state.
Patients supported by methods that certainly maintain enough blood circulation and oxygenation for sustaining life during stopped heartbeat and breathing, such as cardiopulmonary bypass, are not customarily considered clinically dead. All parts of the body except the heart and lungs continue to function normally. Clinical death occurs only if machines providing sole circulatory support are turned off, leaving the patient in a state of stopped blood circulation.
Certain surgeries for cerebral aneurysms or aortic arch defects require that blood circulation be stopped while repairs are performed. This deliberate temporary induction of clinical death is called circulatory arrest. It is typically performed by lowering body temperature to between 18 °C and 20 °C (64 and 68 °F) and stopping the heart and lungs. This state is called deep hypothermic circulatory arrest. At such low temperatures most patients can tolerate the clinically dead state for up to 30 minutes without incurring significant brain injury. [27] Longer durations are possible at lower temperatures, but the usefulness of longer procedures has not been established yet. [28]
Controlled clinical death has also been proposed as a treatment for exsanguinating trauma to create time for surgical repair. [29]
Death was historically believed to be an event that coincided with the onset of clinical death. It is now understood that death is a series of physical events, not a single one, and determination of permanent death is dependent on other factors beyond simple cessation of breathing and heartbeat. [11]
Clinical death that occurs unexpectedly is treated as a medical emergency. CPR is initiated. In a United States hospital, a Code Blue is declared and Advanced Cardiac Life Support procedures used to attempt to restart a normal heartbeat. This effort continues until either the heart is restarted, or a physician determines that continued efforts are useless and recovery is impossible. If this determination is made, the physician pronounces legal death and resuscitation efforts stop.
If clinical death is expected due to terminal illness or withdrawal of supportive care, often a Do Not Resuscitate (DNR) or "no code" order is in place. This means that no resuscitation efforts are made, and a physician or nurse may pronounce legal death at the onset of clinical death.[ citation needed ]
A patient with working heart and lungs who is determined to be brain dead can be pronounced legally dead without clinical death occurring. However, some courts have been reluctant to impose such a determination over the religious objections of family members, such as in the Jesse Koochin case. [30] Similar issues were also raised by the case of Mordechai Dov Brody, but the child died before a court could resolve the matter. [31] Conversely, in the case of Marlise Muñoz, a hospital refused to remove a brain dead woman from life support machines for nearly two months, despite her husband's requests, because she was pregnant. [32]

Cardiac arrest is when the heart stops beating. It is a medical emergency that, without immediate medical intervention, will result in cardiac death within minutes. When it happens suddenly, it is called sudden cardiac arrest. Cardiopulmonary resuscitation (CPR) and possibly defibrillation are needed until further treatment can be provided. Cardiac arrest results in a rapid loss of consciousness, and breathing may be abnormal or absent.

Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest. It is recommended in those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.

Hypothermia is defined as a body core temperature below 35.0 °C (95.0 °F) in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe hypothermia, there may be hallucinations and paradoxical undressing, in which a person removes their clothing, as well as an increased risk of the heart stopping.

Drowning is a type of suffocation induced by the submersion of the mouth and nose in a liquid. Most instances of fatal drowning occur alone or in situations where others present are either unaware of the victim's situation or unable to offer assistance. After successful resuscitation, drowning victims may experience breathing problems, vomiting, confusion, or unconsciousness. Occasionally, victims may not begin experiencing these symptoms until several hours after they are rescued. An incident of drowning can also cause further complications for victims due to low body temperature, aspiration of vomit, or acute respiratory distress syndrome.
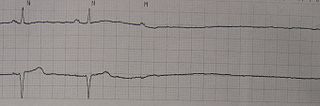
Asystole is the absence of ventricular contractions in the context of a lethal heart arrhythmia. Asystole is the most serious form of cardiac arrest and is usually irreversible. Also referred to as cardiac flatline, asystole is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.

Suspended animation is the temporary slowing or stopping of biological function so that physiological capabilities are preserved. It may be either hypometabolic or ametabolic in nature. It may be induced by either endogenous, natural or artificial biological, chemical or physical means. In its natural form, it may be spontaneously reversible as in the case of species demonstrating hypometabolic states of hibernation. When applied with therapeutic intent, as in deep hypothermic circulatory arrest (DHCA), usually technologically mediated revival is required.
Pulseless electrical activity (PEA) refers to cardiac arrest in which the electrocardiogram shows a heart rhythm that should produce a pulse, but does not. Pulseless electrical activity is found initially in about 55% of people in cardiac arrest.
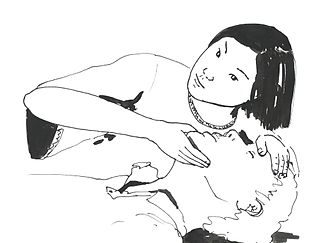
ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.
Deep hypothermic circulatory arrest (DHCA) is a surgical technique that induces deep medical hypothermia. It involves cooling the body to temperatures between 20 °C (68 °F) to 25 °C (77 °F), and stopping blood circulation and brain function for up to one hour. It is used when blood circulation to the brain must be stopped because of delicate surgery within the brain, or because of surgery on large blood vessels that lead to or from the brain. DHCA is used to provide a better visual field during surgery due to the cessation of blood flow. DHCA is a form of carefully managed clinical death in which heartbeat and all brain activity cease.
The history of cardiopulmonary resuscitation (CPR) can be traced as far back as the literary works of ancient Egypt. However, it was not until the 18th century that credible reports of cardiopulmonary resuscitation began to appear in the medical literature.
Targeted temperature management (TTM) previously known as therapeutic hypothermia or protective hypothermia is an active treatment that tries to achieve and maintain a specific body temperature in a person for a specific duration of time in an effort to improve health outcomes during recovery after a period of stopped blood flow to the brain. This is done in an attempt to reduce the risk of tissue injury following lack of blood flow. Periods of poor blood flow may be due to cardiac arrest or the blockage of an artery by a clot as in the case of a stroke.
The Arctic Sun Temperature Management System is a non-invasive targeted temperature management system. It modulates patient temperature by circulating chilled water in pads directly adhered to the patient's skin. Using varying water temperatures and a computer algorithm, a patient's body temperature can be better controlled. It is produced by Medivance, Inc. of Louisville, Colorado.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.
Sam Parnia is a British associate professor of Medicine at the NYU Langone Medical Center where he is also director of research into cardiopulmonary resuscitation. In the United Kingdom, he is director of the Human Consciousness Project at the University of Southampton. Parnia is known for his work on near-death experiences and cardiopulmonary resuscitation.
Slow code refers to the practice in a hospital or other medical centre to purposely respond slowly or incompletely to a patient in cardiac arrest, particularly in situations for which cardiopulmonary resuscitation (CPR) is thought to be of no medical benefit by the medical staff. The related term show code refers to the practice of a medical response that is medically futile, but is attempted for the benefit of the patient's family and loved ones. However, the terms are often used interchangeably.
Extracorporeal cardiopulmonary resuscitation is a method of cardiopulmonary resuscitation (CPR) that passes the patient's blood through a machine in a process to oxygenate the blood supply. A portable extracorporeal membrane oxygenation (ECMO) device is used as an adjunct to standard CPR. A patient who is deemed to be in cardiac arrest refractory to CPR has percutaneous catheters inserted into the femoral vein and artery. Theoretically, the application of ECPR allows for the return of cerebral perfusion in a more sustainable manner than with external compressions alone. By attaching an ECMO device to a person who has acutely undergone cardiovascular collapse, practitioners can maintain end-organ perfusion whilst assessing the potential reversal of causal pathology, with the goal of improving long-term survival and neurological outcomes.
Emergency Preservation and Resuscitation (EPR) is an experimental medical procedure where an emergency department patient is cooled into suspended animation for an hour to prevent incipient death from ischemia, such as the blood loss following a shooting or stabbing. EPR uses hypothermia, drugs, and fluids to "buy time" for resuscitative surgery. If successful, EPR may someday be deployed in the field so that paramedics can suspend and preserve patients for transport.
Lance B. Becker is an American physician and academic, specializing in emergency medicine and treatment for cardiac arrest, currently at Northwell Health. He is the chairman of the department of emergency medicine at North Shore University Hospital, as well as chair and professor of emergency medicine at Hofstra Northwell School of Medicine.
Benjamin S. Abella is an American physician, emergency medicine practitioner, internist, academic and researcher. He is a Professor and Vice Chair of Research at University of Pennsylvania’s Department of Emergency Medicine. He directs the Center for Resuscitation Science and the Penn Acute Research Collaboration at the University. He has participated in developing international CPR guidelines.
Post-cardiac arrest syndrome (PCAS) is an inflammatory state of pathophysiology that can occur after a patient is resuscitated from a cardiac arrest. While in a state of cardiac arrest, the body experiences a unique state of global ischemia. This ischemia results in the accumulation of metabolic waste which instigate the production of inflammatory mediators. If return of spontaneous circulation (ROSC) is achieved after CPR, then circulation resumes, resulting in global reperfusion and the subsequent distribution of the ischemia products throughout the body. While PCAS has a unique cause and consequences, it can ultimately be thought of as type of global ischemia-reperfusion injury. The damage, and therefore prognosis, of PCAS generally depends on the length of the patient's ischemic period; therefore the severity of PCAS is not uniform across different patients.