Cytopathology is a branch of pathology that studies and diagnoses diseases on the cellular level. The discipline was founded by George Nicolas Papanicolaou in 1928. Cytopathology is generally used on samples of free cells or tissue fragments, in contrast to histopathology, which studies whole tissues. Cytopathology is frequently, less precisely, called "cytology", which means "the study of cells".

A biopsy is a medical test commonly performed by a surgeon, interventional radiologist, or an interventional cardiologist. The process involves extraction of sample cells or tissues for examination to determine the presence or extent of a disease. The tissue is then fixed, dehydrated, embedded, sectioned, stained and mounted before it is generally examined under a microscope by a pathologist; it may also be analyzed chemically. When an entire lump or suspicious area is removed, the procedure is called an excisional biopsy. An incisional biopsy or core biopsy samples a portion of the abnormal tissue without attempting to remove the entire lesion or tumor. When a sample of tissue or fluid is removed with a needle in such a way that cells are removed without preserving the histological architecture of the tissue cells, the procedure is called a needle aspiration biopsy. Biopsies are most commonly performed for insight into possible cancerous or inflammatory conditions.
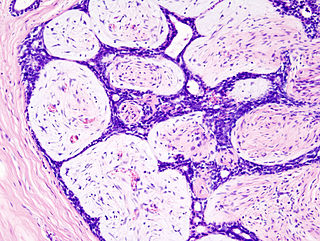
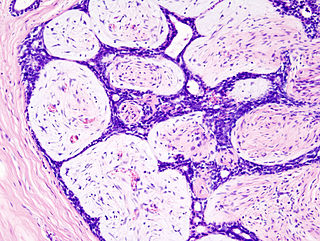
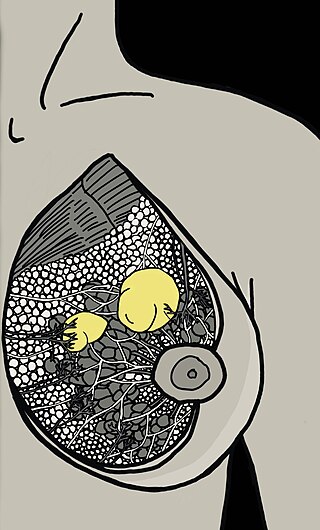
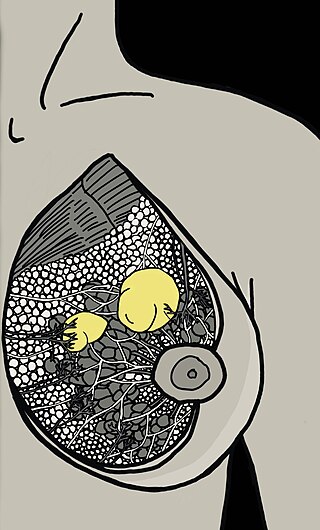
Fibroadenomas are benign breast tumours characterized by an admixture of stromal and epithelial tissue. Breasts are made of lobules and ducts. These are surrounded by glandular, fibrous and fatty tissues. Fibroadenomas develop from the lobules. The glandular tissue and ducts grow over the lobule to form a solid lump.

Fine-needle aspiration (FNA) is a diagnostic procedure used to investigate lumps or masses. In this technique, a thin, hollow needle is inserted into the mass for sampling of cells that, after being stained, are examined under a microscope (biopsy). The sampling and biopsy considered together are called fine-needle aspiration biopsy (FNAB) or fine-needle aspiration cytology (FNAC). Fine-needle aspiration biopsies are very safe minor surgical procedures. Often, a major surgical biopsy can be avoided by performing a needle aspiration biopsy instead, eliminating the need for hospitalization. In 1981, the first fine-needle aspiration biopsy in the United States was done at Maimonides Medical Center. Today, this procedure is widely used in the diagnosis of cancer and inflammatory conditions. Fine needle aspiration is generally considered a safe procedure. Complications are infrequent.

Pleomorphic adenoma is a common benign salivary gland neoplasm characterised by neoplastic proliferation of epithelial (ductal) cells along with myoepithelial components, having a malignant potentiality. It is the most common type of salivary gland tumor and the most common tumor of the parotid gland. It derives its name from the architectural Pleomorphism seen by light microscopy. It is also known as "Mixed tumor, salivary gland type", which refers to its dual origin from epithelial and myoepithelial elements as opposed to its pleomorphic appearance.

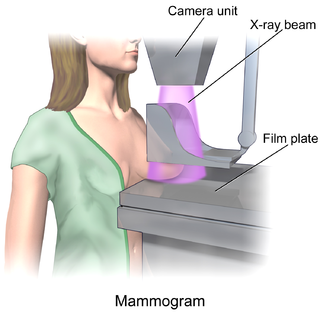
Ductal carcinoma in situ (DCIS), also known as intraductal carcinoma, is a pre-cancerous or non-invasive cancerous lesion of the breast. DCIS is classified as Stage 0. It rarely produces symptoms or a breast lump one can feel, typically being detected through screening mammography. It has been diagnosed in a significant percentage of men.
Fibrocystic breast changes is a condition of the breasts where there may be pain, breast cysts, and breast masses. The breasts may be described as "lumpy" or "doughy". Symptoms may worsen during certain parts of the menstrual cycle due to hormonal stimulation. These are normal breast changes, not associated with cancer.

Surgical pathology is the most significant and time-consuming area of practice for most anatomical pathologists. Surgical pathology involves gross and microscopic examination of surgical specimens, as well as biopsies submitted by surgeons and non-surgeons such as general internists, medical subspecialists, dermatologists, and interventional radiologists.

A breast cyst is a cyst, a fluid-filled sac, within the breast. One breast can have one or more cysts. They are often described as round or oval lumps with distinct edges. In texture, a breast cyst usually feels like a soft grape or a water-filled balloon, but sometimes a breast cyst feels firm.

Thyroid nodules are nodules which commonly arise within an otherwise normal thyroid gland. They may be hyperplastic or tumorous, but only a small percentage of thyroid tumors are malignant. Small, asymptomatic nodules are common, and often go unnoticed. Nodules that grow larger or produce symptoms may eventually need medical care. A goitre may have one nodule – uninodular, multiple nodules – multinodular, or be diffuse.
Stereotactic biopsy, also known as stereotactic core biopsy, is a biopsy procedure that uses a computer and imaging performed in at least two planes to localize a target lesion in three-dimensional space and guide the removal of tissue for examination by a pathologist under a microscope. Stereotactic core biopsy makes use of the underlying principle of parallax to determine the depth or "Z-dimension" of the target lesion.

Mammotome is a Cincinnati, OH based company who pioneered a vacuum-assisted breast biopsy (VAC) device that uses image guidance such as x-ray, ultrasound and/or MRI to perform breast biopsies. A biopsy using a Mammotome® device can be done on an outpatient basis with a local anesthetic. The Mammotome brand is sold in over 45 different countries throughout the world.

Fat necrosis is a form of necrosis that is caused by the action of lipases on adipocytes.
The term nonpuerperal mastitis describes inflammatory lesions of the breast (mastitis) that occur unrelated to pregnancy and breastfeeding.

Atypical ductal hyperplasia (ADH) is the term used for a benign lesion of the breast that indicates an increased risk of breast cancer.

A breast mass, also known as a breast lump, is a localized swelling that feels different from the surrounding tissue. Breast pain, nipple discharge, or skin changes may be present. Concerning findings include masses that are hard, do not move easily, are of an irregular shape, or are firmly attached to surrounding tissue.

Breast ultrasound is a medical imaging technique that uses medical ultrasonography to perform imaging of the breast. It can be performed for either diagnostic or screening purposes and can be used with or without a mammogram. In particular, breast ultrasound may be useful for younger women who have denser fibrous breast tissue that may make mammograms more challenging to interpret.
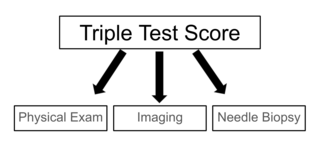
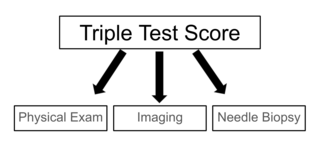
The triple test score is a diagnostic tool for examining potentially cancerous breasts. Diagnostic accuracy of the triple test score is nearly 100%. Scoring includes using the procedures of physical examination, mammography and needle biopsy. If the results of a triple test score are greater than five, an excisional biopsy is indicated.
Breast hematoma is a collection of blood within the breast. It arises from internal bleeding (hemorrhage) and may arise due to trauma or due to a non-traumatic cause.
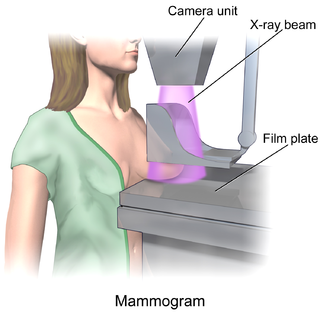
In medicine, breast imaging is a sub-speciality of diagnostic radiology that involves imaging of the breasts for screening or diagnostic purposes. There are various methods of breast imaging using a variety of technologies as described in detail below. Traditional screening and diagnostic mammography uses x-ray technology and has been the mainstay of breast imaging for many decades. Breast tomosynthesis is a relatively new digital x-ray mammography technique that produces multiple image slices of the breast similar to, but distinct from, computed tomography (CT). Xeromammography and galactography are somewhat outdated technologies that also use x-ray technology and are now used infrequently in the detection of breast cancer. Breast ultrasound is another technology employed in diagnosis and screening that can help differentiate between fluid filled and solid lesions, an important factor to determine if a lesion may be cancerous. Breast MRI is a technology typically reserved for high-risk patients and patients recently diagnosed with breast cancer. Lastly, scintimammography is used in a subgroup of patients who have abnormal mammograms or whose screening is not reliable on the basis of using traditional mammography or ultrasound.