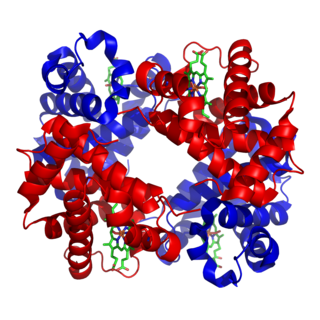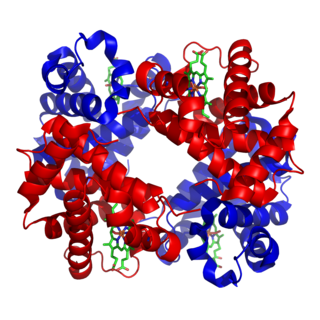
Hemoglobin is a protein containing iron that facilitates the transport of oxygen in red blood cells. Almost all vertebrates contain hemoglobin, with the sole exception of the fish family Channichthyidae. Hemoglobin in the blood carries oxygen from the respiratory organs to the other tissues of the body, where it releases the oxygen to enable aerobic respiration which powers the animal's metabolism. A healthy human has 12 to 20 grams of hemoglobin in every 100 mL of blood. Hemoglobin is a metalloprotein, a chromoprotein, and globulin.

Hemoglobinopathy is the medical term for a group of inherited blood disorders involving the hemoglobin, the protein of red blood cells. They are single-gene disorders and, in most cases, they are inherited as autosomal co-dominant traits.

Hematochezia is a form of blood in stool, in which fresh blood passes through the anus while defecating. It differs from melena, which commonly refers to blood in stool originating from upper gastrointestinal bleeding (UGIB). The term derives from Greek αἷμα ("blood") and χέζειν. Hematochezia is commonly associated with lower gastrointestinal bleeding, but may also occur from a brisk upper gastrointestinal bleed. The difference between hematochezia and rectorrhagia is that rectal bleeding is not associated with defecation; instead, it is associated with expulsion of fresh bright red blood without stools. The phrase bright red blood per rectum is associated with hematochezia and rectorrhagia.

Fetal hemoglobin, or foetal haemoglobin is the main oxygen carrier protein in the human fetus. Hemoglobin F is found in fetal red blood cells, and is involved in transporting oxygen from the mother's bloodstream to organs and tissues in the fetus. It is produced at around 6 weeks of pregnancy and the levels remain high after birth until the baby is roughly 2–4 months old. Hemoglobin F has a different composition than adult forms of hemoglobin, allowing it to bind oxygen more strongly; this in turn enables the developing fetus to retrieve oxygen from the mother's bloodstream, which occurs through the placenta found in the mother's uterus.
Obstetrical bleeding is bleeding in pregnancy that occurs before, during, or after childbirth. Bleeding before childbirth is that which occurs after 24 weeks of pregnancy. Bleeding may be vaginal or less commonly into the abdominal cavity. Bleeding which occurs before 24 weeks is known as early pregnancy bleeding.

Neonatal jaundice is a yellowish discoloration of the white part of the eyes and skin in a newborn baby due to high bilirubin levels. Other symptoms may include excess sleepiness or poor feeding. Complications may include seizures, cerebral palsy, or kernicterus.

Blood in stool looks different depending on how early it enters the digestive tract—and thus how much digestive action it has been exposed to—and how much there is. The term can refer either to melena, with a black appearance, typically originating from upper gastrointestinal bleeding; or to hematochezia, with a red color, typically originating from lower gastrointestinal bleeding. Evaluation of the blood found in stool depends on its characteristics, in terms of color, quantity and other features, which can point to its source, however, more serious conditions can present with a mixed picture, or with the form of bleeding that is found in another section of the tract. The term "blood in stool" is usually only used to describe visible blood, and not fecal occult blood, which is found only after physical examination and chemical laboratory testing.

In humans, the circulatory system is different before and after birth. The fetal circulation is composed of the placenta, umbilical blood vessels encapsulated by the umbilical cord, heart and systemic blood vessels. A major difference between the fetal circulation and postnatal circulation is that the lungs are not used during the fetal stage resulting in the presence of shunts to move oxygenated blood and nutrients from the placenta to the fetal tissue. At birth, the start of breathing and the severance of the umbilical cord prompt various changes that quickly transform fetal circulation into postnatal circulation.

The Kleihauer–Betke ("KB") test, Kleihauer–Betke ("KB") stain, Kleihauer test or acid elution test is a blood test used to measure the amount of fetal hemoglobin transferred from a fetus to a mother's bloodstream. It is usually performed on Rh-negative mothers to determine the required dose of Rho(D) immune globulin (RhIg) to inhibit formation of Rh antibodies in the mother and prevent Rh disease in future Rh-positive children. It is named after Enno Kleihauer and Klaus Betke who described it in 1957.

2,3-Bisphosphoglyceric acid (2,3-BPG), also known as 2,3-diphosphoglyceric acid (2,3-DPG), is a three-carbon isomer of the glycolytic intermediate 1,3-bisphosphoglyceric acid (1,3-BPG).

Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.

Hemoglobin variants are different types of hemoglobin molecules, by different combinations of its subunits and/or mutations thereof. Hemoglobin variants are a part of the normal embryonic and fetal development. They may also be pathologic mutant forms of hemoglobin in a population, caused by variations in genetics. Some well-known hemoglobin variants, such as sickle-cell anemia, are responsible for diseases and are considered hemoglobinopathies. Other variants cause no detectable pathology, and are thus considered non-pathological variants.
Hemoglobin Barts, abbreviated Hb Barts, is an abnormal type of hemoglobin that consists of four gamma globins. It is moderately insoluble, and therefore accumulates in the red blood cells. Hb Barts has an extremely high affinity for oxygen, so it cannot release oxygen to the tissue. Therefore, this makes it an inefficient oxygen carrier. As an embryo develops, it begins to produce alpha-globins at weeks 5–6 of development. When both of the HBA1 and HBA2 genes which code for alpha globins becomes dysfunctional, the affected fetuses will have difficulty in synthesizing a functional hemoglobin. As a result, gamma chains will accumulate and form four gamma globins. These gamma globins bind to form hemoglobin Barts. It is produced in the disease alpha-thalassemia and in the most severe of cases, it is the only form of hemoglobin in circulation. In this situation, a fetus will develop hydrops fetalis and normally die before or shortly after birth, unless intrauterine blood transfusion is performed.

Percutaneous umbilical cord blood sampling (PUBS), also called cordocentesis, fetal blood sampling, or umbilical vein sampling is a diagnostic genetic test that examines blood from the fetal umbilical cord to detect fetal abnormalities. Fetal and maternal blood supply are typically connected in utero with one vein and two arteries to the fetus. The umbilical vein is responsible for delivering oxygen rich blood to the fetus from the mother; the umbilical arteries are responsible for removing oxygen poor blood from the fetus. This allows for the fetus’ tissues to properly perfuse. PUBS provides a means of rapid chromosome analysis and is useful when information cannot be obtained through amniocentesis, chorionic villus sampling, or ultrasound ; this test carries a significant risk of complication and is typically reserved for pregnancies determined to be at high risk for genetic defect. It has been used with mothers with immune thrombocytopenic purpura.

Hemoglobin subunit alpha, Hemoglobin, alpha 1, is a hemoglobin protein that in humans is encoded by the HBA1 gene.

Hemoglobin subunit gamma-2 is a protein that in humans is encoded by the HBG2 gene.

Hemoglobin subunit gamma-1 is a protein that in humans is encoded by the HBG1 gene.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
Hereditary persistence of fetal hemoglobin (HPFH) is a benign condition in which increased fetal hemoglobin production continues well into adulthood, disregarding the normal shutoff point after which only adult-type hemoglobin should be produced.
Fetal-maternal haemorrhage is the loss of fetal blood cells into the maternal circulation. It takes place in normal pregnancies as well as when there are obstetric or trauma related complications to pregnancy.