History
A 54-year-old man with alcoholic cirrhosis hospitalized for liver transplantation presented with a 4-week history of an enlarging ulcer on the left cheek (Fig. 1). His post-transplant course was complicated by septic shock in the setting of ischemic colitis, vancomycin-resistant Enterococcus bacteremia, and Saccharomyces cerevisiae fungemia. Relevant medications included tacrolimus and hydrocortisone for post-transplant immunosuppression, and gentamycin, ampicillin-sulbactam, and amphotericin B for antimicrobial coverage. A biopsy of the ulcer bed and tissue culture were performed, and a bedside scraping of the ulcer bed contents was obtained to aid in diagnosis (Figs. 2, 3, and 4).
Figure 1.
Clinical features, necrotic ulcer on the cheek
Figure 2.
Gram stain of ulcer contents
Figure 3.
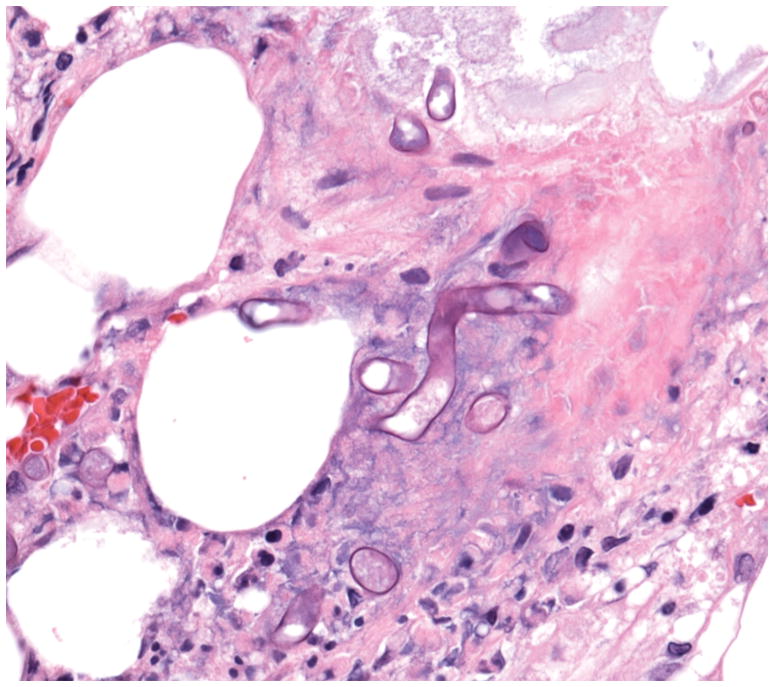
Biopsy specimen, hematoxylin-eosin stain ×40
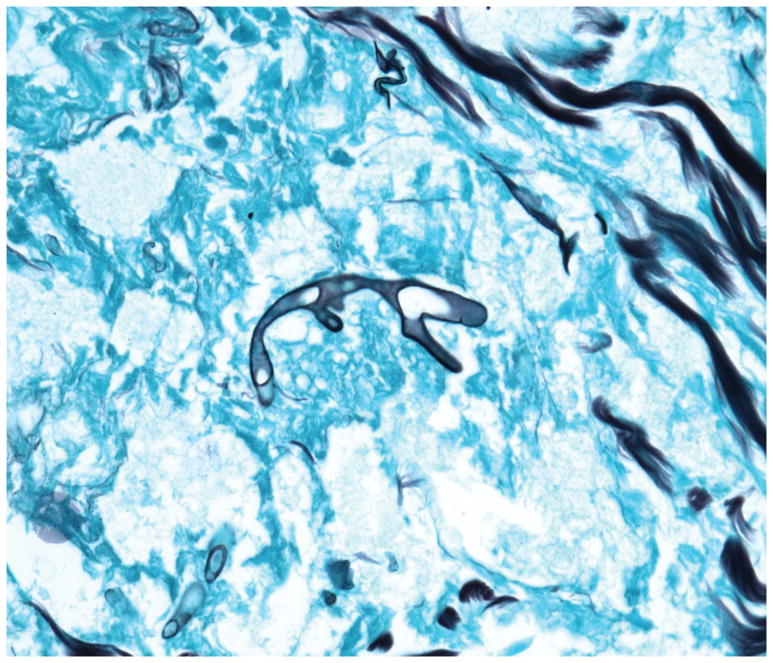
Figure 4.
Biopsy specimen, Grocott’s methenamine silver stain
Diagnosis cutaneous mucormycosis
Discussion
Gram stain of the bedside scraping revealed fungal elements with broad, ribbon-like hyphae (Fig. 2). Histopathology demonstrated suppurative and granulomatous inflammation in the dermis and subcutaneous tissue with broad, non-septate hyphae that stained with Grocott’s methenamine silver (Figs. 3, and 4). Tissue culture confirmed the diagnosis of mucormycosis, rhizopus species. There was no evidence of sinopulmonary involvement. Unfortunately, the patient’s clinical status deteriorated and he died from multi-organ failure.
Mucormycosis has emerged as an important opportunistic fungal infection associated with high mortality rates. The majority of cases are caused by the genera Rhizopus.1 Primary infections may be rhinocerebral, pulmonary, gastrointestinal, or cutaneous, while hematogenous spread may occur in immunocompromised hosts. Direct inoculation, contaminated dressings, surgery, burns, and trauma are associated with primary cutaneous infection.1 The clinical presentation of skin infection is variable, and lesions typically manifest as an indurated plaque that rapidly evolves to necrosis. Other presentations include cellulitis, periorbital edema which may be unilateral, purpuric lesions, and tender nodules, ulcers, or plaques.1 Common risk factors for infection are hematologic malignancy, neutropenia, poorly controlled diabetes, and immunosuppressive medications.2 Treatment with voriconazole and caspofungin, which have no activity against mucormycosis, have also been implicated as risk factors.2 One study demonstrated localization to the skin in 57% of cases of healthcare-associated mucormycosis.3 Prompt diagnosis and treatment of invasive mucormycosis is crucial given the high mortality rate, which may range from 48–71% among solid organ transplantation (SOT) recipients.2 Treatment is multifaceted and should include extensive surgical debridement, antifungal therapy with amphotericin B or azoles, and correction of the underlying immunosuppression or metabolic abnormalities, when feasible.1
The differential diagnosis for a non-healing ulcer in an immunocompromised host includes bacterial infections such as necrotizing cellulitis and ecthyma gangrenosum, atypical mycobacterial infections, dimorphic and other opportunistic fungal infections, chronic herpetic infections, cutaneous malignancies such as squamous cell carcinoma (SCC) for which the risk is disproportionately increased in immunosuppressed patients,4 and inflammatory conditions including pyoderma gangrenosum and medium vessel vasculitides such as granulomatosis with polyangiitis.
Performing a biopsy with tissue culture for common and uncommon pathogens is essential in evaluating non-healing soft tissue ulcers in immunosuppressed patients. This is especially important for SOT recipients, for whom rates of postoperative skin infections are high (55–97%).5 Furthermore, bedside diagnostic techniques such as gram stain, Tzanck smear, acid-fast stains, and potassium hydroxide stains, as well as touch preparations of biopsy specimens may aid in the prompt diagnosis of potentially life-threatening viral, bacterial, fungal, or protozoan infections. Several reports have demonstrated the utility of touch preparations in the diagnosis of invasive cutaneous infections including mucormycosis,6 and multiple stains may highlight fungal organisms including potassium hydroxide, periodic acid–Schiff, Gomori methenamine silver, and gram stain as seen in our case. Dermatologists should be familiar with these bedside diagnostic procedures to aid in rapidly identifying infectious organisms and to allow for early intervention as culture results may not be available for several days.
Footnotes
Financial Disclosures/Conflicts of interest: Ms. Coleman has funding support by the NIH for her Yale School of Medicine Medical Student Fellowship. The remaining authors have no relevant disclosures.
References
- 1.Castrejon-Perez AD, Welsh EC, Miranda I, Ocampo-Candiani J, Welsh O. Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304–311. doi: 10.1590/abd1806-4841.20176614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh N, Aguado JM, Bonatti H, Forrest G, Gupta KL, Safdar N, et al. Zygomycosis in Solid Organ Transplant Recipients: A Prospective, Matched Case-Control Study to Assess Risks for Disease and Outcome. J Infect Dis. 2009;200:1002–11. doi: 10.1086/605445. [DOI] [PubMed] [Google Scholar]
- 3.Rammaert B, Lanternier F, Zahar J-R, Dannaoui E, Bougnoux M-E, Lecuit M, et al. Healthcare-Associated Mucormycosis. Clin Infect Dis. 2012;54:S44–54. doi: 10.1093/cid/cir867. [DOI] [PubMed] [Google Scholar]
- 4.Herrero JI, España A, Quiroga J, Sangro B, Pardo F, Alvárez-Cienfuegos J, et al. Nonmelanoma skin cancer after liver transplantation. Study of risk factors. Liver Transplant. 2005;11:1100–6. doi: 10.1002/lt.20525. [DOI] [PubMed] [Google Scholar]
- 5.Wisgerhof HC, Edelbroek JRJ, de Fijter JW, Feltkamp MCW, Willemze R, Bouwes Bavinck JN. Trends of skin diseases in organ-transplant recipients transplanted between 1966 and 2006: a cohort study with follow-up between 1994 and 2006. Br J Dermatol. 2010;162:390–6. doi: 10.1111/j.1365-2133.2009.09529.x. [DOI] [PubMed] [Google Scholar]
- 6.Antonov NK, Tang R, Grossman ME. Utility of touch preparation for rapid diagnosis of cutaneous mucormycosis. JAAD Case Rep. 2015;1:175–77. doi: 10.1016/j.jdcr.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]