Abstract
Background The origin and estimated death toll of the 1918–1919 epidemic are still debated. Europe, one of the candidate sites for pandemic emergence, has detailed pandemic mortality information.
Objective To determine the mortality impact of the 1918 pandemic in 14 European countries, accounting for approximately three‐quarters of the European population (250 million in 1918).
Methods We analyzed monthly all‐cause civilian mortality rates in the 14 countries, accounting for approximately three‐quarters of the European population (250 million in 1918). A periodic regression model was applied to estimate excess mortality from 1906 to 1922. Using the 1906–1917 data as a training set, the method provided a non‐epidemic baseline for 1918–1922. Excess mortality was the mortality observed above this baseline. It represents the upper bound of the mortality attributable to the flu pandemic.
Results Our analysis suggests that 2·64 million excess deaths occurred in Europe during the period when Spanish flu was circulating. The method provided space variation of the excess mortality: the highest and lowest cumulative excess/predicted mortality ratios were observed in Italy (+172%) and Finland (+33%). Excess‐death curves showed high synchrony in 1918–1919 with peak mortality occurring in all countries during a 2‐month window (Oct–Nov 1918).
Conclusions During the Spanish flu, the excess mortality was 1·1% of the European population. Our study highlights the synchrony of the mortality waves in the different countries, which pleads against a European origin of the pandemic, as was sometimes hypothesized.
Keywords: Death statistics, epidemiology, influenza pandemic, mortality
Introduction
The first pandemic reportedly occurred in 412 BC, 1 , 2 and the first attributed to influenza in 1580. 2 , 3 Since then, 31 influenza pandemics have been described; the five most recent in 1889, 1900, 1918, 1957 and 1968, 1 , 2 , 3 , 4 , 5 were separated respectively by 11, 18, 39 and 11 years. 6
The present threat of a new influenza pandemic is at the origin of renewed interest in the 1918 Spanish flu, as it was undoubtedly the most deadly influenza pandemic in modern history. Recently, Murray et al. extrapolated, in their paper published in 2006, the potential global pandemic influenza mortality occurring in 2004, based on data from the 1918–1920 influenza pandemic. 7
However, the exact death toll of the 1918 pandemic remains very imprecise. A first American report in 1927 suggested that the main 1918–1919 wave was responsible for 21 millions of deaths worldwide. 8 A revised estimation of influenza pandemic mortality given in 1991 was 24·7–39·3 million, 9 and another published in 2002 even set the death toll up to 100 million to take into account the lack of data in a large part of the world. 10
The lack of reliable mortality data in a large part of the world leads to reliance on anecdotal evidence and extrapolation of mortality rates for entire countries from punctual information obtained in highly specific settings. 11 , 12 Concerning Europe, we are aware of only three published papers reporting estimates of the mortality burden. 7 , 9 , 10
Herein, we analyzed the mortality data obtained during the pandemic, in 14 European countries, which accounted for 75% of the European population in 1918.
Methods
Monthly all‐cause deaths of civilians 1906–1936 were obtained from a book published, 13 in 1954, by the French National Institute of Demographic Study, which compiled official demographic and vital statistics from several countries, including 14 European countries. For each country, all‐cause death counts were available on a monthly basis, except for England and Wales, for which only quarterly data are available. The observed data were standardized to mortality rates per 10 000 inhabitants using the corresponding yearly population‐count estimates.
We used a periodic equation to model the monthly baseline mortality rate (B t) of years 1906–1922: 14
with, respectively, n = 12 or n = 4 when monthly or quarterly data were analyzed. In this model, the baseline mortality rate depends on time t through a constant term α0, a secular trend α1, annual predictors γ1 and δ1, semiannual predictors γ2 and δ2 and an error term εt.
The unknown parameters were estimated at maximum likelihood from the fit of a linear regression to data from a ‘training’ period, extending from 1906 to 1917. The estimation was based on the time series truncated from the values observed during the epidemic periods, 15 defined as the 3 consecutive month period with the highest incidence. More precisely, from each annual August 1–July 31 window, we removed the trimester with the highest mortality to take into account seasonal influenza, and the associated annual excess mortality. The August–July period was used because seasonal influenza epidemics occur from fall to spring in Europe.
The baseline model described above was extrapolated to the years 1918–1922. We defined excess‐mortality periods as those starting when observed mortality exceeded the upper limit of the prediction interval [threshold = E (B t) + 1·96 × sd (e t)], for at least 2 consecutive months (one trimester for England and Wales) and ending when the observed mortality fell below the upper limit of the prediction interval. Excess mortality was calculated as the difference between observed and expected baseline deaths during the excess‐mortality period (Figure 1). Cumulative excess mortality was determined throughout the entire pandemic period, 1918–1919.
Figure 1.
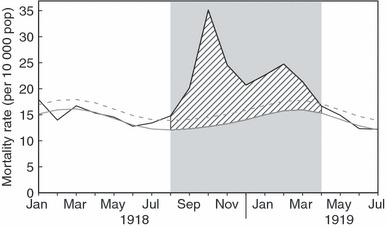
Methods: calculation of excess mortality (France). The cross‐hatched area represents excess mortality, calculated as the difference between observed (black line) and predicted (continuous gray line) mortality, from the beginning of the pandemic period (light gray shading; first month during which observed deaths exceeded the pandemic threshold, dashed gray line) until the end (first month during which observed deaths fell below the pandemic threshold).
For Finland, we subtracted from excess deaths, the 30 000 deaths attributed to the Finnish civil war (January–May 1918). Data for the civilian mortality rates in Germany presented a step pattern for the period 1914–1918, probably reflecting mismatched definitions of population counts and deaths as a result of changing geographical borders. Therefore, we first replaced the linear trend of mortality rates during 1914–1918 by those of the surrounding years (1906–1913 and 1919–1936), and obtained excess mortality as described above.
We also compared the excess mortality in each of the 14 countries during the 1918–1919 pandemic with the excess mortality during the rest of the years (1906–1917; 1920–1922) to determine how worse the 1918 period was compared with those seasons.
All statistical calculations were obtained with r Software. 16
Results
Cumulative excess deaths during the 1918–1919 period were 1·98 million in 14 countries in Europe accounting for ∼75% of the population, an increase of 86% more deaths from baseline. Extrapolating that figure to the rest of Europe, the estimated total mortality in Europe during the 1918 pandemic would be 2·64 (≅1·98/0·75) million deaths, i.e. 1·1% of the entire population estimated at 250 million in 1918. 17
Excess mortality was found to be strongly country dependent. The highest cumulative excess/predicted mortality ratio was observed in Italy (+172%) during the pandemic period (peaked in October 1918), following by Bulgaria and Portugal (+102% each), Spain (+87%), the Netherlands (+84%), Sweden (+74%), Germany (+73%), Switzerland (+69%), France (+66%), Norway (+65%), Denmark (+58%), Scotland (+57%) and England and Wales (+55%), with the lowest ratio being seen in Finland (+33%)(Table 1). The highest excess‐mortality rate (per 10 000 inhabitants) cumulated throughout the entire excess‐mortality period was observed in Portugal (233/10 000 inhabitants), followed by Italy, Spain, Bulgaria, Switzerland, Finland, France, Germany, Sweden, Netherlands, Norway, England and Wales, Scotland and Denmark (Figure 2).
Table 1.
Excess mortality in 14 European countries
| Country | Pandemic period | Cumulative excess deaths n (%)* | Expected mortality | |
|---|---|---|---|---|
| Start | End | |||
| Finland | 1/1918 | 6/1919** | 24771 (+33) | 74667 |
| England and Wales | 10/1918 | 4/1919 | 153152 (+55) | 280507 |
| Scotland | 10/1918 | 4/1919 | 20879 (+57) | 36699 |
| Denmark | 10/1918 | 4/1919** | 10650 (+58) | 18465 |
| Norway | 9/1918 | 5/1919 | 14465 (+65) | 22091 |
| France | 8/1918 | 4/1919 | 237509 (+66) | 360686 |
| Switzerland | 7/1918 | 6/1919** | 29995 (+69) | 43536 |
| Germany | 3/1918 | 1/1919** | 426574 (+73) | 581243 |
| Sweden | 9/1918 | 5/1919 | 38453 (+74) | 51849 |
| The Netherlands | 10/1918 | 5/1919 | 41337 (+84) | 49066 |
| Spain | 6/1918 | 2/1919** | 252121 (+87) | 290531 |
| Portugal | 3/1918 | 6/1919 | 135600 (+102) | 133039 |
| Bulgaria | 3/1918 | 1/1919 | 51156 (+102) | 50015 |
| Italy | 8/1918 | 2/1919 | 544288 (+172%) | 317350 |
| Total 14 countries | 1980950 (+86%) | 2309744 | ||
*Represents the excess mortality calculated, based on expected baseline mortality.
**Existence of a later peak in April 1920 (not taken into account to calculate excess deaths throughout the pandemic period).
Figure 2.

Excess‐mortality rates* cumulated throughout the entire excess‐mortality period in each European country. Note the north–south gradient in the progressively darker shades of gray, *(/10 000 inhabitants).
Overall, the excess mortality found during the pandemic was 3·5 times higher than the excess mortality found in the rest of the 1906–1922 period. This ratio ranged between 1·6 (Finland) and 6·1 (Portugal) (Table 2).
Table 2.
Excess mortality (%) comparison between the 1918–1919 pandemic periods and the rest of the years (1906–1917; 1920–1922) in each of the 14 countries
| Country | Pandemic period (1) | Seasonal period (2) | Ratio (1)/(2) | ||
|---|---|---|---|---|---|
| Average | Range | SD | |||
| France | 66·0 | 22·8 | 13–61 | 7·9 | 2·9 |
| Germany | 73·0 | 32·8 | 18–56 | 9·1 | 2·2 |
| Switzerland | 69·0 | 19·7 | 12–42 | 6·9 | 3·5 |
| The Netherlands | 84·0 | 26·4 | 12–57 | 13·9 | 3·2 |
| Norway | 65·0 | 14·0 | 8–32 | 5·7 | 4·6 |
| Denmark | 58·0 | 20·0 | 13–30 | 4·7 | 2·9 |
| Finland | 33·0 | 20·3 | 10–41 | 10·0 | 1·6 |
| Sweden | 74·0 | 15·1 | 9–32 | 6·2 | 4·9 |
| Bulgaria | 102·0 | 49·4 | 34–109 | 24·8 | 2·1 |
| Spain | 87·0 | 16·4 | 12–26 | 3·6 | 5·3 |
| Portugal | 102·0 | 16·8 | 14–24 | 3·5 | 6·1 |
| Italy | 172·0 | 31·9 | 15–147 | 32·0 | 5·4 |
| Scotland | 57·0 | 23·3 | 12–57 | 12·3 | 2·4 |
| England and Wales | 55·0 | 17·5 | 13–22 | 6·4 | 3·1 |
We found a statistically significant negative correlation (Spearman’s rank correlation ρ = −0·66; P = 0·013) between excess mortality and latitude (Figure 2), meaning that northern countries experienced significantly less mortality, while Southern Europe suffered significantly more excess deaths. No relationship between excess mortality and longitude was observed (Spearman’s rank correlation ρ = −0·20; P = 0·48).
Countries were clustered according to their mortality patterns (Figure 3): countries with one sharp mortality peak (e.g. Portugal, Spain, Italy, Bulgaria), countries with two major peaks (e.g. Switzerland, Scotland, Netherlands and France), country with several successive peaks (only Finland).
Figure 3.
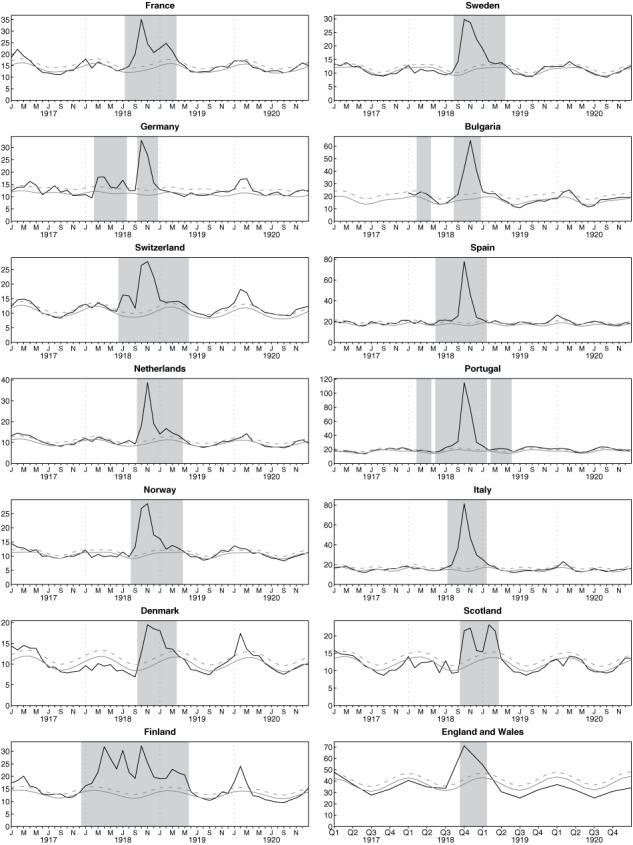
Monthly (or trimesterly) mortality rate* (ordinate) in 14 European countries from 1917 to 1921 (abscise). Lines and shading are as defined in the legend to Figure 1, *(/10 000 inhabitants).
Excess mortality was time dependent: the start and stop months of the excess‐mortality period varied across the continent and occurred in four waves (Figure 4, Table 1). Moreover, an early first wave of deaths, occurring between March 1918 and July 1918, was observed in six countries (Bulgaria, Portugal, Germany, Finland, Switzerland and Spain) (Figure 4). Importantly, the excess‐death curves could be temporally superposed, albeit not of the same intensity, for 1918–1919, with mortality peaking in all countries within a 2‐month window (October–November 1918, Figure 3), defined as the second wave (Figure 4). In five countries (Spain, Denmark, Finland, Germany and Switzerland), a late peak between January 1920 and April 1920 was recorded. That fourth wave in 1920 was not taken into account in estimating the cumulative excess‐death rates for the entire pandemic period.
Figure 4.

Geographic spread of the excess‐mortality peaks.
Discussion–Conclusion
The limitation of any study focused on mortality burden at the epoch of the Spanish pandemic depends on the exhaustiveness of the data. During this period, vital statistics were sometimes described as being in their infancy. 18 Official reports could be incomplete (destruction of archives or late recording). 10 Data were often scattered in various places or sources, making their collection for analyses difficult. This is the reason why earlier publications were based on various documents dating from 1918 to 1919 (medical journals, daily newspapers and archives). In this study we took advantage of the existence of vital statistics compiled in European countries by demographers, using a homogeneous method. 13 Thus, we retrieved reliable all‐cause mortality data from 14 European countries. We used the information available on the monthly variations of death figures to estimate the pandemic mortality burden, based on the values of a 12 years ‘learning’ period with seasonal influenza. Three previous assessments of the European pandemic burden were published. 7 , 9 , 10 These assessments were done on different sets of European countries. None of them took account of the seasonal variations of mortality. The recent estimates provided by Murray et al., 7 were for example computed by simply making the difference between the 1918 and 1920 yearly mortality data and the values observed in the preceding and succeeding 3‐year periods. The comparison of the datasets used in the different mortality assessments, and the results obtained, are shown in Figure 5. There is a good agreement between the four reports in a majority of countries. The largest observed differences between estimates were in Germany, Italy and Spain. The changes in borders and the mass population movements related to World War 1 may be one reason for these discrepancies. For example, in Germany, we checked that using the raw data (not corrected for the mismatches of populations and deaths) would have lowered our estimation of 426 574 to ∼340 000, changing the excess mortality estimate from 73 to 67%. In total, however, the agreement between estimates are more remarkable than the discrepancies. For example, the total European burden was estimated at 2 300 000 in the two first reports, published in 1991 and 2002, based respectively on 18 countries 9 and 21 countries, 10 at 2 005 569 deaths in the paper from Murray et al. 7 (total of their 13 European values) versus 1 980 950 deaths in this report.
Figure 5.

Comparison of published mortality estimates in Europe (number of deaths) during the 1918–1919 influenza pandemic. Circle: Johnson and Mueller (J); Dark circle: Ansart et al. (A); square: Patterson and Pyle (P); triangle: Murray et al. (M).
As the 14 European countries we have studied in this paper represented 75% of the European population at that time, one can deduce that ∼2·6 million excess deaths (1·1% of the total population) occurred in Europe during the period when Spanish flu was circulating. American excess deaths during the same period were estimated at 550 000 (corresponding to 0·65% of the American population) by Glezen WP. 19 However, Johnson‐Mueller 10 put the US figure at 675 000 deaths and more recently Murray et al. 7 at only 400 000 deaths (0·47% of the total population). Whatever is taken as estimation of the American pandemic death burden, it is well below the European estimations we provide and others have provided. A possible explanation is that, at the end of WW1, Europe was characterised by massive civilian and army movements, a health care system put at its minimum and frail populations. This has very likely heavily impacted the European death toll. Finally, we measure the indirect impact of the influenza virus on the mortality. Herein, we analyzed all‐cause mortality and not only influenza or pneumonia deaths. Indeed, we were obliged to base our estimation on the available monthly data on concerned total mortality, not influenza–and–pneumonia (P&I) mortality However, there is a striking linear relationship between the overall annual influenza–and–pneumonia mortality records, for each of the 11 countries where such data were available, and the total number of excess deaths (Figure 6). This is consistent with the hypothesis that P&I mortality is a relatively constant proportion of the total number of deaths, and supports our use of the total number of excess deaths to quantify the death toll of the pandemic.
Figure 6.
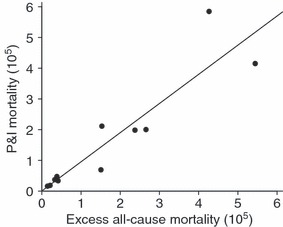
P&I‐deaths plotted versus all‐cause excess mortality in 11 European countries*. Spearman’s rank correlation ρ = 0·94; P < 10−4. *Germany, Spain, France, Italy, Norway, Netherlands, Portugal, Sweden, Switzerland, England and Wales and Scotland.
There was a high level of variability between the excess of mortality experienced in the 14 countries we studied, with a minimal value of 33% in Finland and a maximal value of 172% in Italy. Ninety years later, the reasons for this variability are difficult to investigate. We pointed out that there was a clear north–south gradient, but did not find a rationale for this gradient. All factors that can be related to the mortality burden such as the existence of co‐infectious diseases, especially bacterial pneumonia and tuberculosis, or socio‐economic status were unlikely to have a north–south gradient. Possible geographic determinants of the influenza mortality are cold temperature and vitamin D deficiency relative to low sunlight exposure, but they would have implied a higher mortality in northern countries, not the opposite as we observed.
We observed a high degree of synchronism in Europe, with the highest mortality peak occurring in all countries within a 2‐month window (Oct–Nov 1918) (3, 4). All but two countries (Denmark and Italy) experienced at least a two‐wave pattern. In addition to this common feature, six countries had an earlier first wave of excess mortality before October 1918 (Bulgaria, Portugal, Germany, Finland, Switzerland and Spain) and five countries (Spain, Denmark, Finland, Germany and Switzerland) had one late excess‐mortality waves in February and March 1920. The very peculiar profile of mortality in Finland could be explained by their civil war that caused 30 000 deaths in early 1918 (that could not be excluded directly from our analysis because of their unknown spatiotemporal distribution).
A fourth wave having occurred in the early spring 1920 similar to the one we found was reported before in specific settings. 10 Including 6 additional months in the calculation of excess mortality (until July 1920), would have increased the burden estimates as follows: ∼405 800 (+153 744) deaths in Spain, ∼60 500 (+5768) in Finland, ∼13 600 (+3044) in Denmark, ∼510 200 (+83 663) in Germany and ∼39 000 (+9080) in Switzerland.
Where the 1918 pandemic first emerged is still being debated. A recent analysis of the 1918 H1N1 genome failed to single out a particular location. 20 , 21 The origin has been successively proposed in Asia, 8 in a British army post in France in 1916, 22 , 23 in USA, 8 , 21 , 24 , 25 or in Spain. 24 An Asian origin could explain the pandemic starting in summer. 26 The European origin was not supported by Taubenberger et al. in their 1997 report on the sequence of the 1918‐virus genome extracted from autopsy samples (obtained from the Armed Forces Institute of Pathology in Washington, DC) of 28 US servicemen who died of the flu during their military service. 27 Our findings can provide clues as to the origin of the pandemic and do not make plausible an European origin: indeed, if the pandemic would have started somewhere in Europe, we would have expected to see a spatiotemporal spread outwards from this hypothetical origin, while the data show that all the European countries reached simultaneously their epidemic peaks.
Potential conflict in interest
None reported.
Author contributions
All authors contributed to the study and agree with the contents of the manuscript. Conceived and designed the study: SA, AJV, PYB, CP. Collected the data: SA. Analyzed the data: SA, CP, PYB, AJV. Contributed materials, analysis tools: FC, AF. Wrote the paper: SA, AJV. Participated in the interpretation of data: FC, AF. Revised the paper critically: CP, PYB, FC, AF.
Acknowledgement
This work was supported by EU grant INFTRANS.
References
- 1. Potter CW. Chronicle of influenza pandemics; in Nicholson KG, Webster RG, Hay AJ. (eds): Textbook of Influenza. Oxford: Blackwell Science Ltd, 1998; 3–18. [Google Scholar]
- 2. Potter CW. A history of influenza. J Appl Microbiol 2001; 91:572–579. [DOI] [PubMed] [Google Scholar]
- 3. Noble GR. Epidemiological and clinical aspects of influenza; in Beare AS. (ed): Basic and Applied Influenza Research. Boca Raton, Florida: CRC Press, 1982: 11–50. [Google Scholar]
- 4. Kilbourne ED. Influenza pandemics of the 20th century. Emerg Infect Dis 2006; 12:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Oxford JS. Influenza A pandemics of the 20th century with special reference to 1918: virology, pathology and epidemiology. Rev Med Virol 2000; 10:119–133. [DOI] [PubMed] [Google Scholar]
- 6. Dowdle WR. Influenza pandemic periodicity, virus recycling, and the art of risk assessment. Emerg Infect Dis 2006; 12:34–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Murray CJ, Lopez AD, Chin B, Feehan D, Hill KH. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: a quantitative analysis. Lancet 2006; 368:2211–2218. [DOI] [PubMed] [Google Scholar]
- 8. Jordan EO. Epidemic Influenza: A Survey. Chicago: American Medical Association, 1927. [Google Scholar]
- 9. Patterson DK, Pyle GF. The geography and mortality of the 1918 influenza pandemic. Bull Hist Med 1991; 65:4–21. [PubMed] [Google Scholar]
- 10. Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med 2002; 76:105–115. [DOI] [PubMed] [Google Scholar]
- 11. Patterson KD, Pyle GF. The diffusion of influenza in sub‐Saharan Africa during the 1918–1919 pandemic. Soc Sci Med 1983; 17:1299–1307. [DOI] [PubMed] [Google Scholar]
- 12. Mills ID. The 1918–1919 influenza pandemic – the Indian experience. Indian Econ Soc Hist Rev 1986; 23:1–36. [DOI] [PubMed] [Google Scholar]
- 13. Bunle H. Le mouvement naturel de la population dans le monde de 1906 à 1936. Paris: Institut National d’Etudes Démographiques, 1954. [Google Scholar]
- 14. Pelat C, Boelle PY, Cowling BJ, et al. Online detection and quantification of epidemics. BMC Med Inform Decis Mak 2007; 7:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Olson DR, Simonsen L, Edelson PJ, Morse SS. Epidemiological evidence of an early wave of the 1918 influenza pandemic in New York City. Proc Nat Acad Sci U S A 2005; 102:11059–11063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. R Development Core Team . A language and environment for statistical computing. Vienna, Austria, 2008; Available at: http://www.R‐project.org . (Accessed 28 June 2006). [Google Scholar]
- 17. Guedel N. L’épidémie de grippe espagnole en 1918–1919 et ses répercussions sur la ville de Lyon. Thèse d’Histoire de la Médecine. Université de Lyon, 1991. [Google Scholar]
- 18. Ammon CE. Grippe espagnole à Genève (1918–1919): souvenirs d’une pandémie (Janvier 2006). Site officiel de l'Etat de Genève. DES. Available at: http://etat.geneve.ch/des/site/sante/grippe‐aviaire‐pandemie/master‐content.jsp?componentId=kmelia839&themeId=3045&pubId=6808. (Accessed 6 March 2009). [Google Scholar]
- 19. Glezen WP. Emerging infections: pandemic influenza. Epidemiol Rev 1996; 18:64–76. [DOI] [PubMed] [Google Scholar]
- 20. Oxford JS, Lambkin R, Sefton A, Daniels R, Elliot A et al. A hypothesis: the conjunction of soldiers, gas, pigs, ducks, geese and horses in northern France during the Great War provided the conditions for the emergence of the “Spanish” influenza pandemic of 1918–1919. Vaccine 2005; 23:940–945. [DOI] [PubMed] [Google Scholar]
- 21. Taubenberger JK, Reid AH, Janczewski TA, Fanning TG. Integrating historical, clinical and molecular genetic data in order to explain the origin and virulence of the 1918 Spanish influenza virus. Philos Trans R Soc Lond B Biol Sci 2001; 356:1829–1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oxford JS. The so‐called Great Spanish Influenza Pandemic of 1918 may have originated in France in 1916. Philos Trans R Soc Lond B Biol Sci 2001; 356:1857–1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Oxford JS, Sefton A, Jackson R, Innes W, Daniels RS et al. World War I may have allowed the emergence of “Spanish” influenza. Lancet Infect Dis 2002; 2:111–114. [DOI] [PubMed] [Google Scholar]
- 24. Barry JM. The Great Influenza: The Epic Story of the Deadliest Plague in History. New York: Viking Penguin, 2004: 546 p. [Google Scholar]
- 25. Taubenberger JK, Morens DM. 1918 influenza: the mother of all pandemics. Emerg Infect Dis 2006; 12:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ammon CE. Spanish flu epidemic in 1918 in Geneva, Switzerland. Euro Surveill 2002; 7:190–192. [DOI] [PubMed] [Google Scholar]
- 27. Taubenberger JK, Reid AH, Krafft AE, Bijwaard KE, Fanning TG. Initial genetic characterization of the 1918 “Spanish” influenza virus. Science 1997; 275:1793–1796. [DOI] [PubMed] [Google Scholar]